A study in Vancouver found an increase in severe, multidrug-resistant (MDR) shigellosis cases and a shift in patient demographics, researchers reported yesterday in Clinical Infectious Diseases.
For the study, a team of researchers from the University of British Columbia conducted a retrospective review of 163 patients diagnosed as having Shigella sonnei infections from 2015 through 2022. Based on clinically observed changes in the populations affected—from men who have sex with men (MSM) to people experiencing homelessness (PEH)— and shifts in antimicrobial susceptibility patterns, they stratified the case-patients into two periods: the historical period (2015 to 2020) and the recent period (2021 to 2022). Severe shigellosis was defined as including hospitalization, bacteremia, or death.
Overall, there were 50 case-patients in the historical period and 113 in the recent period, and the infection rate rose from 8.3 to 56.5 cases per year. A review of patient demographics revealed that 98% of S sonnei infections during the historical period were in MSM, while 77% of infections in the recent period occurred in PEH. A significant increase in severe shigellosis cases was observed in the recent period compared with the historical period (61% vs 14%).
Increased resistance to first- and second-line agents
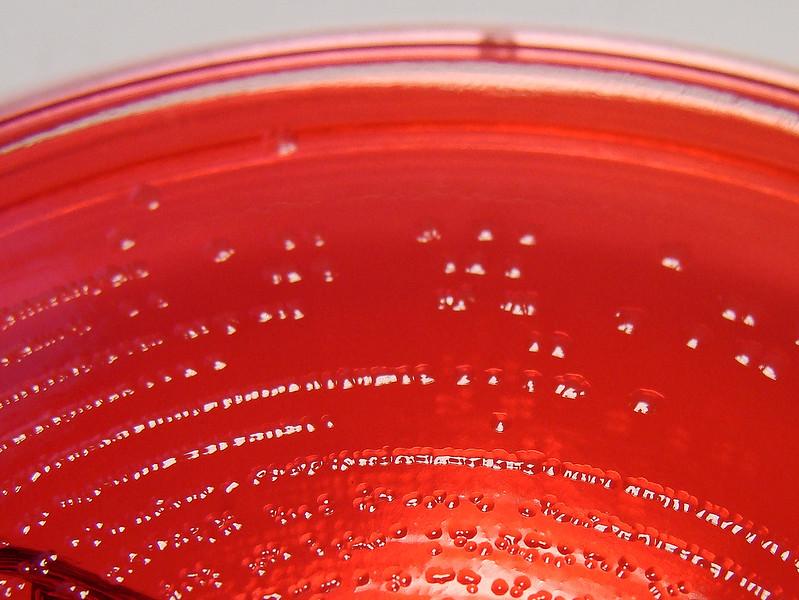
Susceptibility of S sonnei to oral antibiotics also decreased significantly during the recent period. MDR was present in only 11 (22%) of historical isolates, compared with 109 (96%) from the recent period. Whole-genome sequencing of isolates from the recent period revealed the emergence of a dominant clone of MDR S sonnei, 3.6.1.1.2, with resistance to all first- and second-line agents but susceptibility to ceftriaxone.
Shigella is transmitted by the oral-fecal route; via contaminated fomites, food, and water; or by direct person-to-person contact. Although sexual transmission is well-established in MSM, the study authors say transmission among PEH in Vancouver is likely occurring following exposure to fecally contaminated environmental surfaces and hands. A similar shift in patient demographics, driven by similar factors and overlap of the two populations, has been observed in Seattle.
"The introduction of Shigella into congregate living settings (shelters, SROs, etc.) among PEH with limited access to hygiene and sanitation likely created favorable conditions for its widespread transmission," they wrote.
They add that host factors such as malnutrition, history of substance abuse, and associated health issues likely contributed to increased severity of infections in PEH.
"Potential interventions to reduce shigellosis in PEH include improved sanitation and handwashing, improved access to hygiene facilities, optimised nutrition, and, eventually, vaccination against Shigella," the authors concluded.