An analysis of Campylobacter infections in the United States found that their incidence remained stable or decreased from 2012 through 2018, but antibiotic resistance increased, researchers reported today in Open Forum Infectious Diseases.
Using data on laboratory-confirmed Campylobacter jejuni and Campylobacter coli infections from the Foodborne Diseases Active Surveillance Network, researchers with the Centers for Disease Control and Prevention and the California and Tennessee state health departments estimated trends in incidence of infection from 2005 through 2018, adjusting for sex, age, and surveillance changes attributable to culture-independent diagnostics tests. They used a subset of Campylobacter isolates collected by the National Antimicrobial Resistance System to compare changes in resistance to erythromycin and ciprofloxacin over time.
Since 2012, adjusted Campylobacter incidence saw a predicted yearly change of –0.1% (95% credible interval [CrI], -1.1% to 0.9%). Incidence was lower among men than women and higher among children under 5 compared with other age-groups. Among 2,499 linked records in 2017-2018, the median patient age was 40.2 years, 54.8% of patients were men, 17.2% were hospitalized, and 0.2% died.
Resistance tied to international travel
The percentage of resistant infections increased from 24.5% in 2005-2016 to 29.7% in 2017-2018 for ciprofloxacin and from 2.6% to 3.3% for erythromycin—increases of 21% and 27%, respectively. People with recent international travel had higher odds than non-travelers of having isolates resistant to erythromycin (adjusted odds ratio [aOR], 1.7; 95% confidence interval [CI]. 1.3 to 2.1) and to ciprofloxacin (aOR varied from 1.7 to 10.6 by race/ethnicity).
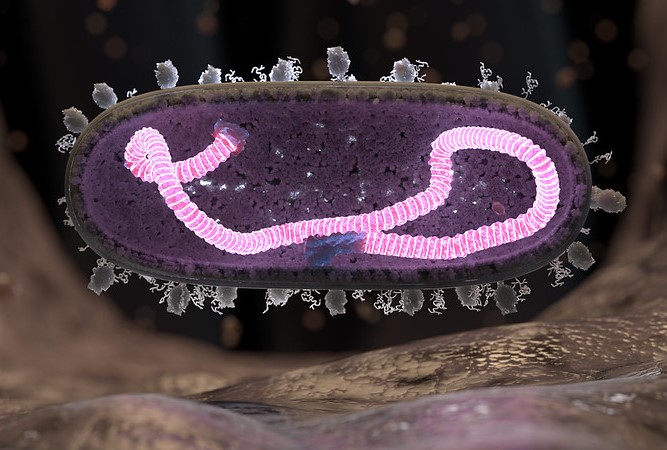
Campylobacter is the most common cause of bacterial diarrheal disease in the United States and is associated with consumption of undercooked poultry, animal contact, and international travel. Although illness usually resolves without antibiotics, the study authors note that rising resistance is a concern because antibiotic treatment can shorten symptoms and be lifesaving in the case of severe infections.
Before beginning empiric treatment, clinicians should consider the patient's risk factors (including travel history).
"Evaluation of antimicrobial use and infection prevention practices could help identify ways to reduce resistant Campylobacter infections," they wrote. "Before beginning empiric treatment, clinicians should consider the patient's risk factors (including travel history) and consider ordering confirmatory diagnostic testing with antibiotic susceptibility testing to guide treatment if indicated."
 mRNA COVID-19 vaccines induced an antibody response in both mothers and babies for at least 6 months after birth, with no adverse outcomes, according to a single-center
mRNA COVID-19 vaccines induced an antibody response in both mothers and babies for at least 6 months after birth, with no adverse outcomes, according to a single-center  A randomized clinical trial found that direct oral penicillin challenge in patients with a low-risk penicillin allergy was non-inferior to the standard-of-care skin test, investigators reported today in JAMA Internal Medicine.
A randomized clinical trial found that direct oral penicillin challenge in patients with a low-risk penicillin allergy was non-inferior to the standard-of-care skin test, investigators reported today in JAMA Internal Medicine.














