US surveillance for candidemia shows a stable to slightly increasing incidence but a rising death rate from 2017 to 2021, likely influenced by overwhelmed healthcare systems amid the pandemic and more patients susceptible to Candida species because of severe COVID-19 infections.
Researchers from the Centers for Disease Control and Prevention (CDC), state public health departments, and healthcare systems tracked candidemia cases and deaths at city or county sites in 10 states for 5 years, publishing the results today in Morbidity and Mortality Weekly Report.
The sites were in California, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, New York, Oregon, and Tennessee.
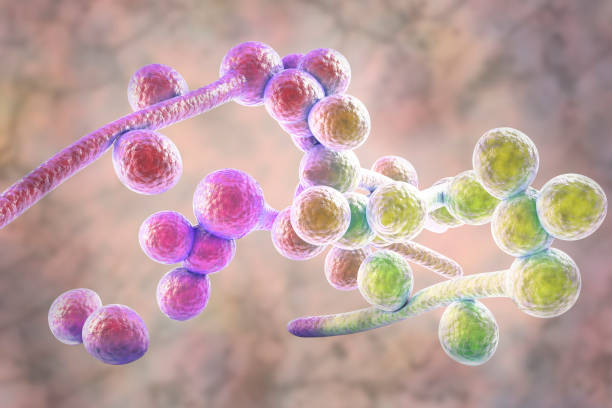
Candidemia, a fungal bloodstream infection caused by Candida yeast, can cause severe illness and death, often in patients who are hospitalized or have a weakened immune system. It is linked to substantial US healthcare costs.
"Candida spp. are a normal component of the gastrointestinal microbiome and can colonize the skin," the researchers wrote. "Candidiasis can be mucocutaneous or invasive; the most common invasive form is Candida bloodstream infection (candidemia), which is among the most frequent health care–associated infections in the United States. Additional forms of invasive candidiasis can occur after dissemination of Candida from the bloodstream to other normally sterile body sites."
Older, Black, male patients at highest risk
Surveillance identified 7,381 candidemia cases, with an incidence of 7.4 cases per 100,000 people. Across age-groups, sexes, racial groups, and surveillance sites, incidence was generally stable or increased slightly, with the lowest overall incidence in 2019 (6.8) and the highest in 2021 (7.9).
The higher mortality rate associated with candidemia during 2020–2021 likely reflects consequences of the COVID-19 pandemic, including strained health care systems and an increased population of patients who were susceptible to candidemia because of COVID-19–related critical illness.
In 2021, candidemia rates were highest in patients aged 65 years and older (22.7 per 100,000) and infants (8.0). Incidence was higher in males (8.7) than in females (7.0) and in Black (12.8) than non-Black patients (5.6).
Incidence was highest in Maryland (14.5), followed by Tennessee (10.1) and Georgia (10.0) and lowest in Oregon (4.8). The proportion of infections categorized as healthcare-related rose from 52.2% in 2017 to 58.0% in 2021. In total, 63.7% of cases occurred in patients with a central venous catheter, 80.7% involved recent systemic antibiotic use, and 9.0% occurred in injection-drug users.
The percentage of patients coinfected with SARS-CoV-2 in the 90 days before or after the index date jumped from 10.4% in 2020 to 17.7% in 2021. Over the study period, the proportion of patients requiring intensive care before the index date climbed from 38.3% to 44.9%. In total, 32.6% of patients died in the hospital of any cause, a rate that rose from 26.8% in 2019 to 36.1% in 2021.
"The higher mortality rate associated with candidemia during 2020–2021 likely reflects consequences of the COVID-19 pandemic, including strained health care systems and an increased population of patients who were susceptible to candidemia because of COVID-19–related critical illness," the authors wrote.
C albicans most common cause
C albicans was responsible for 37.1% of cases overall, followed by C glabrata (30.4%) and C parapsilosis (13.5%), but C glabrata was the most common species in California (38.4%) and Maryland (32.9%). C auris infections, which are especially deadly and often antimicrobial resistant, accounted for 0.4% of cases.
Strict implementation of measures to prevent health care–associated bloodstream infections is important to help prevent candidemia cases.
Therapy consisted of echinocandins (49.8%) or azoles (47.7%). Of the 6,576 Candida isolates with interpretive breakpoints and isolates for testing, 5.6% were fluconazole-resistant, and less than 1% were resistant to echinocandins. Antifungal resistance was consistent across the years for all drugs tested.
"The disproportionate incidence among older adults, males, and Black patients is consistent with previous reports, and the overall incidence of candidemia has not changed substantially compared with previous EIP [CDC Emerging Infections Program] findings based on data collected during 2012–2016 (8.7 per 100,000 population)," the study authors wrote.
"Strict implementation of measures to prevent health care–associated bloodstream infections is important to help prevent candidemia cases," they added. "Health care officials and providers should be vigilant for candidemia as a complication of critical illness."