The Center for Disease Control and Prevention (CDC) vaccine advisory group today recommended the chikungunya vaccine for people ages 18 and older who will be traveling to a country or territory experiencing an outbreak of the disease.
The vote passed with 12 yes votes and 1 abstention.
Last November the Food and Drug Administration (FDA) approved the nation's first chikungunya vaccine, which is a live attenuated vaccine made by Valneva that is given as one intramuscular dose.
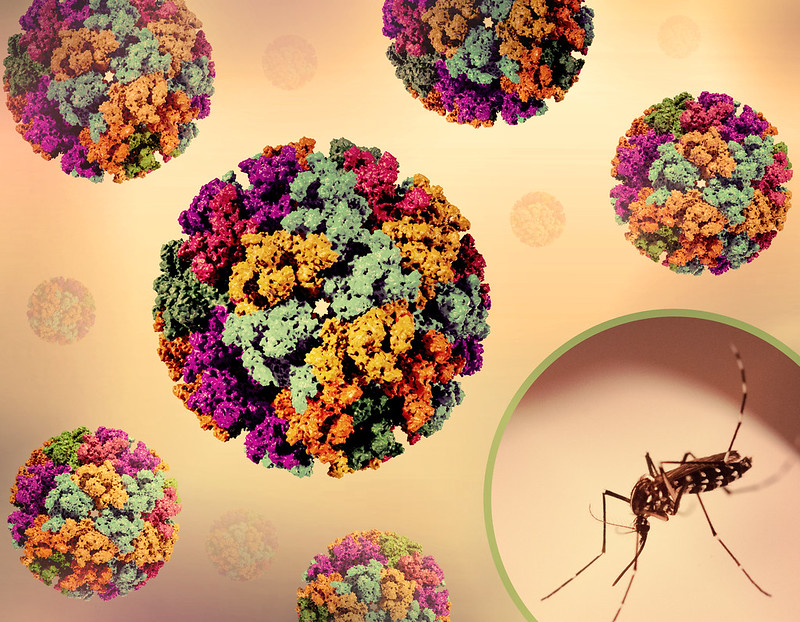
Chikungunya is an emerging health threat that has sickened more than 5 million people over the past 15 years, mainly in areas where the mosquito that carries the virus is endemic. The disease isn't usually fatal but can cause fever, plus debilitating joint pain that can last for months.
As part of ACIP's recommendation, the group also said that use of the vaccine may be considered for certain people traveling to a country or territory where chikungunya has been known to circulate in the past 5 years. They include people older than 65, especially those with underlying health conditions who are likely to have at least moderate exposure to mosquitoes, and people who will be staying in affected areas for 6 months or more.
Group also recommends vaccine for certain lab workers
In a separate vote, which passed unanimously, the group recommended chikungunya vaccination for lab workers who are potentially exposed to the virus.
Infections in lab workers have been rare in the United States. Among the few cases, two involved needlesticks in scientists who were working with mice and one involved a forceps prick in a lab worker who was dissecting mosquitoes, a CDC expert said today.