A new study suggests that kids who develop MIS-C (multisystem inflammatory syndrome in children), a severe complication following COVID-19 infections, may do so because COVID reactivates a latent Epstein-Barr virus (EBV) in their bodies. The study appears in Nature.
For 5 years, researchers have struggled to explain how MIS-C, a severe inflammatory response that mimics symptoms of toxic shock and Kawasaki shock syndromes, can occur in children who seem to recover completely from mild or even asymptomatic COVID infections. Kids with MIS-C typically develop the condition 4 to 8 weeks after SARS-CoV-2 infection.
German researchers say the answer may be in virus-reactive memory T cells, which are triggered by COVID infection.
We’ve now found indications, however, that a resurgence of a second pathogen—Epstein-Barr virus—is responsible for the inflammatory shock.
“We’ve now found indications, however, that a resurgence of a second pathogen—Epstein-Barr virus—is responsible for the inflammatory shock. Put simply, it wakes up from a dormant state because the COVID infection has thrown the child’s immune system in such disarray that it becomes unable to keep the dormant infection in check,” said Tilmann Kallinich, MD, co-senior author of the study, in a press release from Charite hospital in Berlin.
80.7% OF MIS-C patients seropositive for EBV
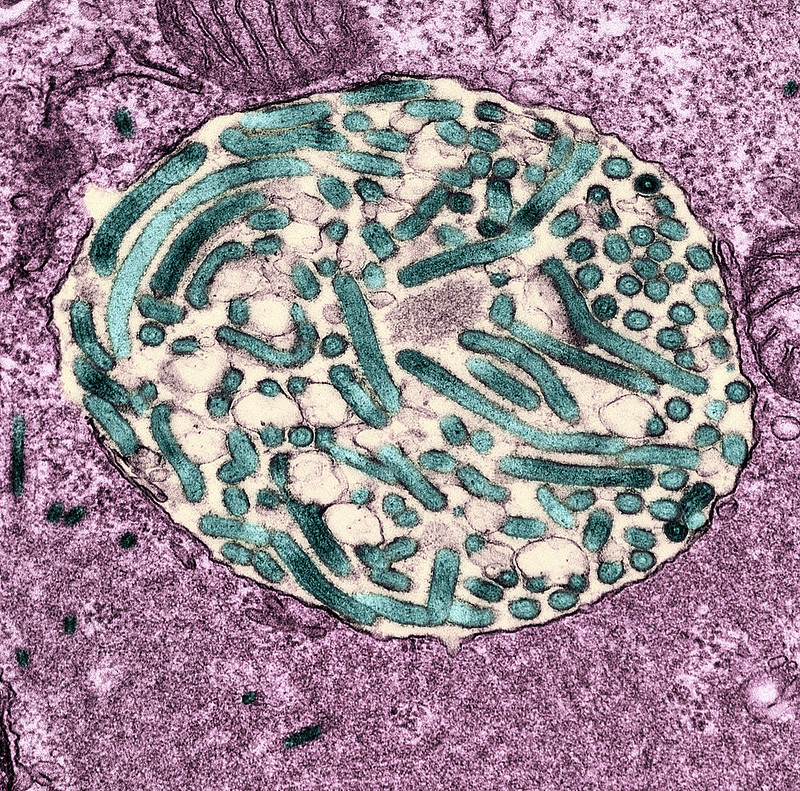
Epstein-Barr is the virus that causes mononucleosis, and while some have symptoms, almost 90% of people are infected, and most never have a symptom, but EBV is dormant in immune cells.
In the study, 145 children aged 2 to 18 years old who had been treated for MIS-C in European hospitals were compared to 105 controls who had COVID-10 but never developed MIS-C. Researchers found that 80.7% of kids with MIS-C had evidence of EBV in blood samples, compared to 56.0% of controls. EBV antibody titers were higher in patients with MIS-C compared with controls and treated patients, the authors said.
They added that COVID may trigger an inflammatory immune response in kids that damages organs.