In US Ebola developments today, joy over a nurse's hospital discharge was tempered with concerns about a hospitalized doctor in New York City who battled the disease in Guinea, as the global response geared up to battle an especially worrisome situation with Mali's first case.
Late yesterday New York City's health department announced that a health worker who returned from West Africa reported a fever and was taken by a special emergency medical service team to Bellevue Hospital, one of several in New York equipped to manage Ebola cases.
A few hours later New York health officials announced that initial tests on the man's samples were positive for Ebola, and the US Centers for Disease Control and Prevention (CDC) said that its confirmation tests were positive for the disease as well. The illness is the fourth detected in the United States and the second linked to exposure in West Africa.
The patient has been identified as Craig Spencer, MD, MPH, a 33-year-old physician from Columbia University who worked with Doctors without Borders (MSF) in Guinea. The CDC said he returned through New York City's JFK Airport on Oct 17 and participated in enhanced screening for all travelers returning from West Africa's outbreak countries.
At a media briefing today, New York authorities said public health officials are tracing the man's contacts and that three close contacts have been quarantined, according to the New York Times. His fever was 100.3°F when he reported it yesterday at 11:00 am, and he is in stable condition. Spencer's doctors are discussing experimental options for treating his infection.
Hazardous materials crews descended on Spencer's apartment to begin decontamination, and public health teams traced his movements in the days before he became ill, the Times reported. Spencer told investigators he started feeling sluggish on Tuesday, when he visited Manhatten's High Line park and ate at a restaurant. On Wednesday he went for a 3-mile jog, took the subway to Brooklyn, went bowling in Williamsburg, and took a taxi back to Manhattan.
Mary Bassett, MD, MPH, New York City's health commissioner, said that, out of an abundance of caution, health officials are working to identify anyone who had contact with Spencer from Oct 21 at 7:00 am, when he first started feeling slightly unwell, the Times reported.
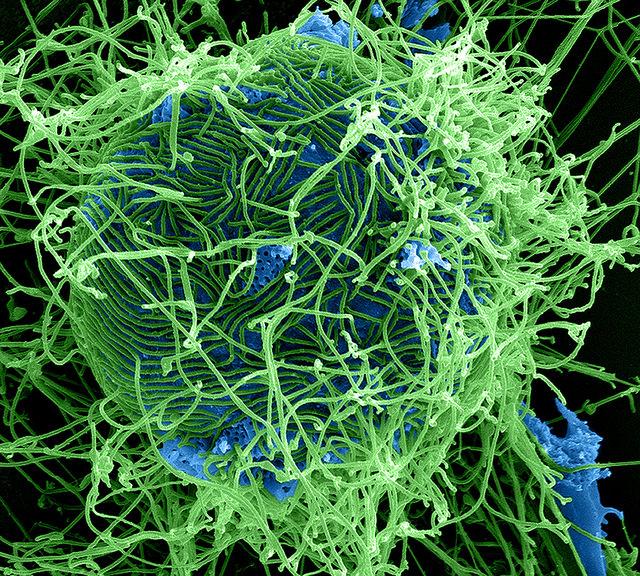
Health officials have emphasized that Ebola spreads only through contact with bodily secretions and that patients don't transmit the virus until they have symptoms.
In a statement late yesterday, MSF said Spencer is the first of its 700 staff deployed so far to West Africa to get sick with Ebola after turning to their home countries. Two other MSF workers were infected with the virus and airlifted out of the region for treatment and have recovered.
MSF said Spencer followed all of its protocols for staff returning to the United States, including twice-daily temperature monitoring, malaria prophylaxis, staying within 4 hours of a hospital with isolation facilities, and immediately contacting MSF if any Ebola symptoms develop.
The organization said he immediately contacted its office in New York after he detected his fever, after which he remained in his apartment until paramedics arrived to take him to Bellevue Hospital. It added that he posed no threat to the public before developing symptoms.
The group said self-quarantine is not warranted or recommended when a person is not displaying symptoms.
Pham discharged from NIH hospital
As New York City's Ebola response kicked into high gear, medical teams at the National Institutes of Health (NIH) Clinical Center in Bethesda, Md., announced that the first nurse infected with Ebola, Nina Pham, has recovered from her infection and was discharged from the hospital.
Pham is one of two Dallas nurses who took care of the nation's first Ebola patient, a Liberian man who died from his illness. Two days ago the family of a second infected nurse, Amber Joy Vinson, announced that tests at Emory University Hospital have shown that she is also free of the virus.
The NIH said on its Twitter feed during a media briefing today that Pham is free of Ebola after five negative tests for the virus. Pham appeared at the briefing and thanked her care teams at the NIH and at Texas Health Presbyterian Hospital in Dallas.
The NIH said she didn't receive any experimental treatments at its facility. However, according to earlier reports during her hospitalization in Dallas she received convalescent serum from Kent Brantly, MD, who recovered from the disease in August.
Pham was first hospitalized in Dallas on Oct 10 after developing a fever. She was one of the 48 identified contacts of the Liberian man who died from the disease, Thomas Eric Duncan. Pham's infection and that of Vinson exposed lapses in personal protective equipment (PPE) protocols that have now been tightened, the CDC has said, along with gaps in hospital Ebola preparedness.
WHO: Mali case poses high exposure risks
Meanwhile, the World Health Organization (WHO) said yesterday that Mali's health ministry has confirmed the country's first Ebola infection and that samples have been sent to a WHO-affiliated laboratory for further testing. The WHO said the girl's symptoms and travel history are worrisome and may have exposed others in Mali to the disease.
The patient is a 2-year-old girl who came from Guinea with her grandmother. The girl's first medical visit in Mali was on Oct 20, when she was seen by a health worker in Kayes, a city of 128,000 in the western part of the country near the border with Senegal.
The girl and her grandmother were hospitalized the next day, and the girl's symptoms included fever, a cough, bleeding from the nose, and blood in the stools. Diagnostic tests were negative for malaria but positive for typhoid fever. Further tests of the girl's samples conducted at Mali's national lab were positive for Ebola yesterday.
The girl has reportedly died from her infection, according to Reuters, which cited an unnamed health official and local radio station reports.
An investigation found that the grandmother traveled from Mali to a funeral in Kissidougou, Guinea. The WHO said it is seeking to confirm media reports that the child's mother had Ebola symptoms before she died.
On Oct 19 the two returned to Mali, with the child bleeding from her nose before they left Guinea, suggesting the girl was symptomatic during travel in Mali. The pair took public transportation to Bamako, Mali's capital, where they remained for 2 hours before continuing on to Kayes. The WHO said multiple exposures occurred while the girl had visible symptoms. "The WHO is treating the situation in Mali as an emergency," the agency said.
The girl is being treated in isolation, and so far the investigation has identified 43 close and unprotected contacts, including 10 health workers who are also being monitored in quarantine.
Mali has acted quickly, and the WHO and the CDC were already in Mali helping with Ebola preparedness efforts, the group said. The staff is now assisting with a surge response to the first Ebola detection in Mali.
Mali is the third West African country outside of the three main outbreak nations to report Ebola related to the outbreak. The WHO recently announced that virus transmission had ended in the other two countries, Nigeria and Senegal.
Congress members question preparedness, quarantine procedures
The two latest developments, especially the New York case, spilled over in a 4-hour US House of Representatives Oversight and Government Reform committee hearing on coordination of the US multiagency response. Today's hearing was especially contentious, compared with the tone of other recent Congressional hearings, coming just a few weeks before midterm elections.
Some of the House members contended that Spencer's infection shows that tightened travel screening steps aren't working and asked why outbreak workers and others aren't required to spend the 21-day fever monitoring period oversees, rather than in the United States.
Rabih Torbay, senior vice president of international operations for International Medical Corps, which has 800 health workers in the outbreak region, said the out-of-country monitoring period would make it difficult to recruit and retain health worker volunteers, considered a key tool in battling the outbreak.
He added that the extra monitoring would increase volunteer commitments from 6 weeks to 9 weeks, interfering with leave time from work and extending the time away from their families. "We can't completely wrap ourselves in a bubble here," he said.
Some legislators said reports that Spencer felt sluggish a few days ago raise questions about whether self-monitoring and self-quarantine are effective.
Deborah Burger, RN, co-president of National Nurses United (NNU), the nation's largest nurses union, told committee members that a team is needed to more formally follow and monitor returning health workers. She said it may be unrealistic to expect health workers to monitor their own health, when they are in the patient role. "They're humans. They're patients," she said.
House members also grilled defense department witnesses on the risk to deployed military members who are in the outbreak countries. Maj Gen James Lariviere, deputy director for political-military affairs in Africa for the US Department of Defense (DoD), said troops won't be providing care to Ebola patients and that strict protocols are in place, such as daily fever checks, hand washing regimens, and avoidance of public contact.
Michael Lumpkin, assistant secretary of defense for the DoD, said 698 troops are in West Africa now, with the ability to reach inaccessible areas. "What looks to be impossible, they made possible," he said, adding that the US military is an interim solution until international capacity mobilizes.
Rep Elijah Cummings, D-Md., the committee's ranking member, said he can understand the emotion of the American people about protecting healthcare workers and military members. "That's serious business," he said, asking the NNU's Burger what more needs to be done to train hospital staff and responders. Burger called for mandatory standards for PPE gear and training.
Darrell Issa, R-Calif., chairman of the committee, said it's important to investigate preparedness lapses in the weeks to come, and he compared the Ebola epidemic to the current terror threat. For both, the problem needs to be addressed at the source, and for Ebola, response sights need to focus on Africa, he added.
See also:
Oct 23 NYC Health media briefing transcript
Oct 23 CDC statement
Oct 24 Times story
Oct 23 MSF statement
Oct 24 NIH press release
Oct 24 WHO statement
Oct 24 Reuters story
Oct 24 US House subcommittee materials