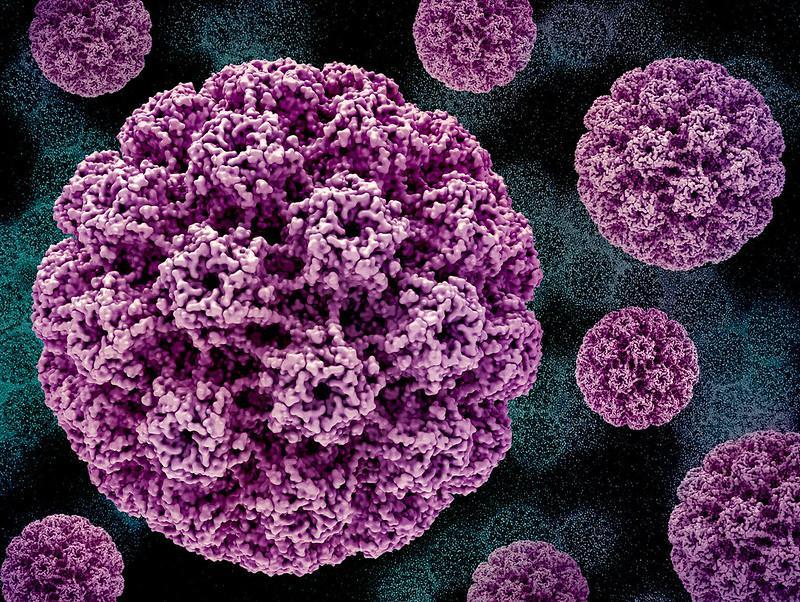
In a new study in JAMA Pediatrics, population-level effectiveness and herd immunity were robust 17 years after human papillomavirus (HPV) vaccine introduction, even in sexually experienced adolescent girls and young women at relatively high risk for HPV who may not have received the full vaccination series.
The study was led by researchers from the Albert Einstein College of Medicine and included data from six studies conducted in Cincinnati of 2,335 adolescent and young adult women between 2006 (the year before the HPV vaccine became available) and 2023.
The participants were 13 to 26 years old at the age of enrollment, with an average age of 18.9 years, and 65.4% were Black and 24.9% were White.
Overall, 79% reported two or more male sexual partners, while half (51%) reported at least one sexually transmitted infection. Multiple partners and sexually transmitted infections are risk factors for HPV, a virus that can cause cervical cancer and genital warts.
Participants were considered vaccinated if they had at least one dose of either the 2-valent, 4-valent, or 9-valent HPV vaccine. All vaccines offered protection against HPV types 16 and 18 (responsible for over 70% of cervical cancers). The 4-valent and 9-vaent vaccines also protect against types 6 and 11, which cause about 90% of genital warts.
Between 2006 and 2023, vaccination rates reached 82%, and researchers found significant drops in infections covered by the 2-valent vaccine (98.4%), the 4-valent (94.2%), and the 9-valent vaccine (75.7%).
Reductions in infection rates were primarily due to the vaccine’s introduction and not because of changes in sexual behavior or other factors.
“Our analysis of the data indicates that those reductions in infection rates were primarily due to the vaccine’s introduction and not because of changes in sexual behavior or other factors,” said Aislinn DeSieghardt, MS, the paper’s first author and clinical research coordinator at Cincinnati Children’s Hospital Medical Center in a press release.
Unvaccinated women saw significant drop in HPV types 16 and 18
Among unvaccinated women included in the study, infections with HPV types 16 and 18 decreased by 71.6%, and infections with HPV types covered in the 4-valent vaccines dropped by 75.8%. The authors said this strong evidence of herd immunity was due to vaccine uptake among both girls and boys in the United States.
“HPV vaccines work remarkably well in a real-world setting, even among women at high risk for HPV and who may not have received all vaccine doses,” said lead author Jessica Kahn, MD, MPH. “We saw clear evidence of herd immunity, meaning when enough people are vaccinated, the vaccine indirectly protects unvaccinated people by reducing overall virus transmission."
In a commentary on the study, the authors said this work shows the significant effect HPV vaccination has had on the US population. In the past 17 years, the HPV vaccine has been administered to more than 59 million women. Before HPV vaccination more than 80% of sexually active Americans acquired HPV in their lifetime.
Now the success seen in the US should be a model for other countries, the authors said.