Influenza infection can boost the likelihood of bacterial pneumonia 100-fold, according to a new study that teased out the interaction between the two diseases.
Increases in pneumonia cases during flu epidemics have been documented over the last two centuries, but different types of studies have yielded inconsistent, puzzling findings about the association between the two illnesses.
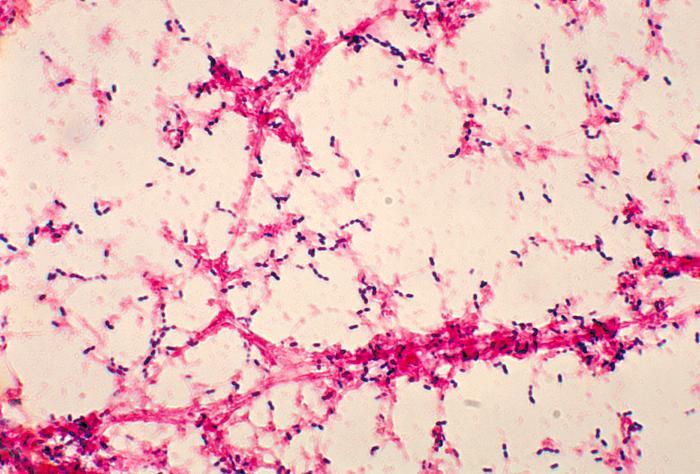
Pathology studies in individual patients have clearly found that secondary bacterial infections are a factor in deadly and severe influenza infections. However, when scientists look at the relationship between the two diseases at the population level, they find no interaction or only a modest link.
A research team from the University of Michigan and their colleagues in Connecticut and Maryland used a computerized model of pneumonia transmission that tested different hypotheses. As they explain today in Science Translational Medicine, they used real flu and pneumonia data in their testing—weekly hospitalizations in Illinois from 1989 to 2009.
They used the model to rank the likelihood of three hypotheses
- That people with pneumonia contribute more to transmission if they recently had flu
- That people with flu are more susceptible to pneumococcal pneumonia
- That flu boosts only the severity of subsequent pneumonia infections.
Results showed no evidence to support the transmission or severity hypotheses. However, the team found strong support for the susceptibility hypothesis—that the heightened risk for pneumonia lasted a week after flu infection.
Pejman Rohani, PhD, an epidemiologist and population ecologist at the University of Michigan School of Public Health and senior author of the study, said in a University of Michigan press release that findings about the nature of the interaction between flu and pneumococcal pneumonia were unequivocal. "Simply put, our analyses identified a short-lived but significant—about 100-fold—increase in the risk of pneumococcal pneumonia following influenza infection."
When the group gauged the fraction of pneumonia cases that could be linked to flu, they found that at the peak of the season, flu infections were responsible for as many as 40% of pneumococcal pneumonia cases. However, on a yearly basis, the magnitude was more subtle, at about 2% to 10% of cases. The team said the lower yearly fraction they found might explain why earlier studies did not detect a connection.
Rohani said in the press release that according to the study the best way to reduce levels of bacterial pneumonia is to urge the public to get both pneumococcal and influenza vaccinations.
In a commentary on the study published in the same issue, Joanne Lello, PhD, a co-infection biology expert at the Cardiff School of Biosciences in Wales, wrote that the researchers have used a well-known model in a new way to address questions about the co-infection dynamics at different levels.
She noted that the team focused on one side of the flu-pneumococcus relationship, but there is evidence from mouse models that flu viral titers are also affected by Streptococcus pneumoniae infection. The current approach could be used to probe the role of pneumococcus infection on flu epidemiology and that variations of the modeling approach could be used to explore other types of co-infections.
The links between parasite infections, infection risks, and host pathology in co-infections are still poorly understood, and the researchers add a new tool for assessment, she wrote, adding that the next step will be to model unidirectional and multidirectional interactions. "Because knowing which parasites drive infection dynamics in a system will help determine how best to target limited resources for efficacious control strategies."
Shrestha S, Foxman B, Weinberger DM, et al. Identifying the interaction between influenza and pneumococcal pneumonia using incidence data. Sci Transl Med 2013 Jun 26;5(191) [Abstract]
Lello J. Coinfection: doing the math. (Editorial) Sci Transl Med 2013 Jun 26;5(191) [Extract]
See also:
Jun 26 University of Michigan press release