 The risk of flu-related intensive care unit (ICU) admission was sevenfold higher in lower middle-income countries (LMICs) than in high-income countries (HICs), according to an analysis yesterday in the Journal of Infectious Diseases.
The risk of flu-related intensive care unit (ICU) admission was sevenfold higher in lower middle-income countries (LMICs) than in high-income countries (HICs), according to an analysis yesterday in the Journal of Infectious Diseases.
The Global Influenza Hospital Surveillance Network conducted the study, the first to evaluate years of global, patient-level data from hospitals to determine geographic differences in flu severity. The analysis included 15,660 patients admitted to 116 hospitals in 22 countries for flu from 2012 through 2019. Of all patients, 72.4% had influenza A, and 27.6% had influenza B.
"Given lack of routine testing for influenza, and the complex pathway by which influenza can exacerbate chronic conditions and lead to severe disease, influenza burden estimates remain uncertain, especially in data-poor settings," the authors wrote.
Comorbidities doubled the risk
After adjustment for patient-level covariates, the risk of flu-related ICU admission was sevenfold higher in LMICs than in HICs. Having two or more underlying medical conditions significantly heightened the likelihood of ICU admission, mechanical ventilation, and in-hospital death (adjusted odds ratios [aORs], 2.40, 2.58, and 1.66, respectively), while female sex was protective against death (aOR, 0.80).
Relative to patients aged 5 to 64 years, those 65 and older had double the odds of death (aOR, 2.18), and those younger than 5 had lower chances of ICU admission, mechanical ventilation, and death (aORs, 0.67, 0.67, and 0.17, respectively).
Delayed care-seeking in LMIC could contribute to the increased severity.
Admission during the 2017-18 flu season increased the risk of ICU admission, mechanical ventilation, and death (aORs, 1.62, 2.15, and 1.37, respectively). Infection with the influenza A H1N1 strain independently predicted ICU admission (aOR, 1.67), mechanical ventilation (aOR, 1.47), and death (aOR, 1.37) compared with influenza A H3N2.
The researchers noted that flu vaccination is generally less available in LMICs. "Moreover, differences in standards of care and/or lack of access to antivirals in LMIC are also a possible explanation," they wrote. "Delayed care-seeking in LMIC could contribute to the increased severity."
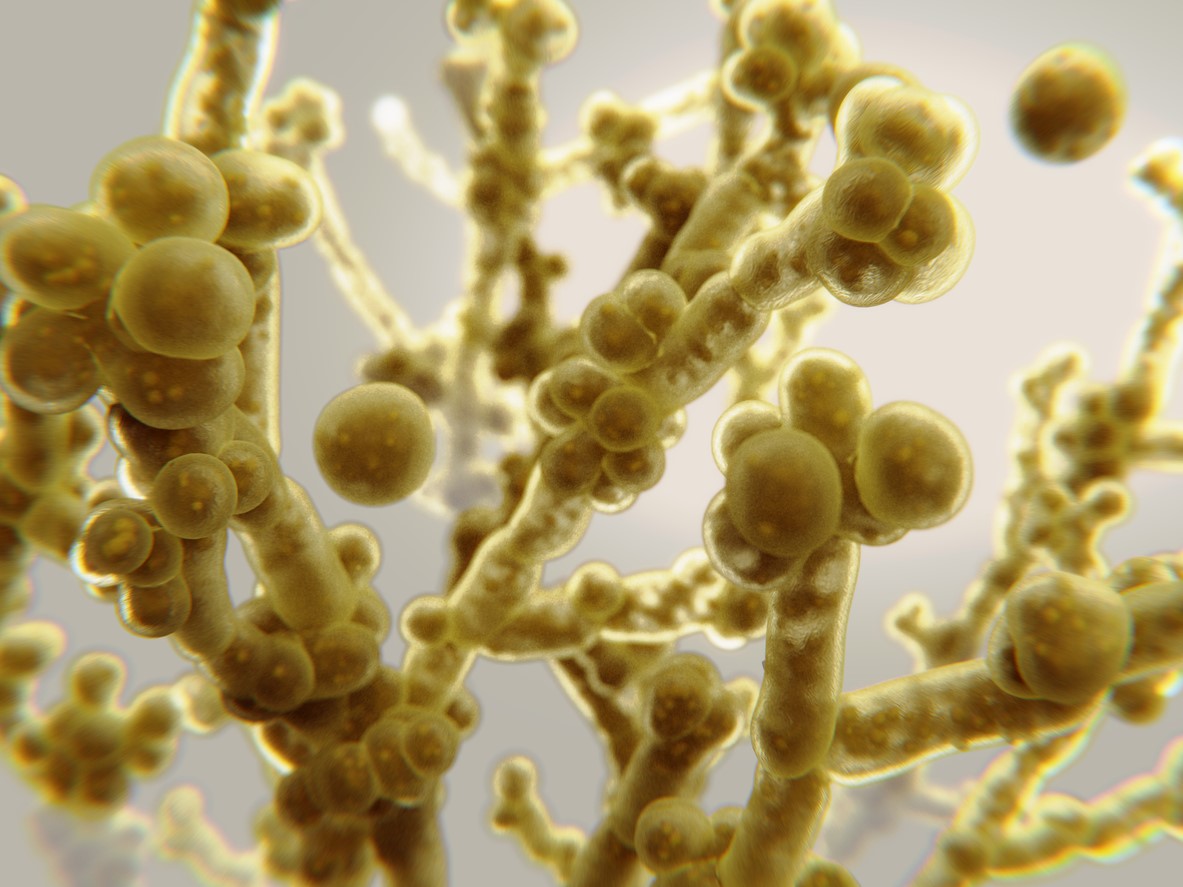 Testing by a team of researchers with the Louis Stokes Cleveland VA Medical Center indicates that sporicidal disinfectants are more effective against the multidrug-resistant fungal pathogen Candida auris than quaternary-ammonium disinfectants, according to a study published today in Infection Control & Hospital Epidemiology.
Testing by a team of researchers with the Louis Stokes Cleveland VA Medical Center indicates that sporicidal disinfectants are more effective against the multidrug-resistant fungal pathogen Candida auris than quaternary-ammonium disinfectants, according to a study published today in Infection Control & Hospital Epidemiology.










