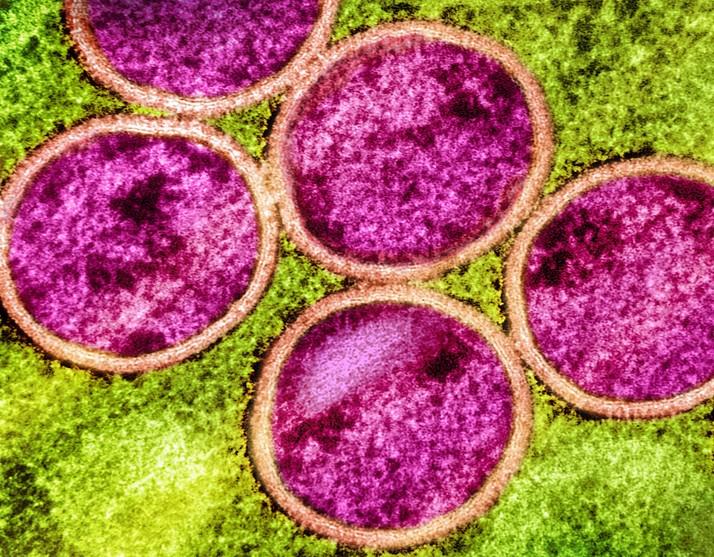
New in Emerging Infectious Diseases is a case history of a 33-year-old man from Baltimore who died from mpox complications, one of the 42 fatal cases documented in the United States during the latest outbreak of the disease, which began last summer.
The case highlights the challenges of using novel therapeutic regimens to treat orthopoxviruses, as well as the complications posed by untreated HIV infection.
Early treatment attempts
The man, who had untreated HIV, first presented to a hospital with a rash, diarrhea, and pain when swallowing. He said his his last sexual contact was with a male partner 10 days prior to hospitalization, with the development of lesions 4 days prior to hospitalization.
The man had 25 to 30 raised lesions across his body, and a viral load of 678,000 copies per milliliter (mL) (ideal range in HIV infection, <20 copies/mL). The patient was initially treated with oral tecovirimat (Tpoxx) at 600 mg twice daily, and discharged after 10 days.
The man was readmitted to a different hospital 48 hours after discharge with worsening fever and rash. He was treated with intravenous tecovirimat, but was unaccepting of his HIV status and refused to begin antiretroviral therapy (ART). He checked himself out of the second hospital against medical advice.
Possible pulmonary involvement
A third hospital admission followed 2 weeks later, as several lesions were now ulcerated and open, and the patient at this point had extreme swelling and pain.
"He declined ART throughout this hospitalization and initially deferred mpox medications," the authors said. "We empirically treated suspected bacterial superinfection with vancomycin and cefepime, which were later transitioned to linezolid and meropenem secondary to worsening leukocytosis and fevers."
He declined ART throughout this hospitalization and initially deferred mpox medications.
Sixty days after his first lesions appeared, the man's rash now involved his left eye and arm. He once again began oral tecovirimat and adjunctive brincidofovir. By day 73, he experienced severe respiratory distress and was intubated. On day 74, the man died of cardiac arrest, and his cause of death was classified as severe monkeypox infection.
The severe case of mpox involved pulmonary illness. Historically, intratracheal monkeypox virus administration in macaques causes rapidly progressive fatal pneumonia, the authors said.
"We lack pathologic evidence, but this patient's lung complications could be secondary to mpox. The role of early imaging and biopsy in identifying those lesions warrants further study," the authors said.
Added complications with HIV
As the global mpox outbreak grew last summer predominantly among men who have sex with men, more links between infection, disease progression, and HIV status have been noted. Patients with untreated or poorly managed HIV tend to have worse clinical outcomes with mpox, thus ART should always be initiated upon mpox diagnosis, the authors write.
"Barriers to HIV treatment are still prevalent and include poverty, behavioral health disorders, and substance use disorders. Fear of living with HIV and lack of awareness regarding the benefits of ART also play a role," the authors said, which was likely seen in this case.
In a related development, the Centers for Disease Control and Prevention just released a health update warning clinicians of a possible resurgence in mpox cases in the coming months (see today's CIDRAP story). More than 30,000 cases have been documented in the United States, and as summer includes more festivals and public gatherings, officials warn that more cases could occur.