With more than 20 years of research into HIV/AIDS prevention under his belt, Tom Patterson, PhD, knows well the damage that viruses can inflict. The last thing he expected was to be saved by them.
But as Patterson, a professor of psychiatry at the University of California, San Diego (UCSD), lay in a coma in January 2016, his body riddled with a multidrug-resistant Acinetobacter baumannii infection, viruses that infect and destroy bacteria were looking like they might be his only hope. His wife, Steffanie Strathdee, PhD, just had to convince his doctors to give the viruses, known as bacteriophages, a try.
An epidemiologist by training and associate dean of global health sciences at the UCSD School of Medicine, Strathdee also knows a thing or two about infectious diseases. But she didn't know anything about bacteriophage therapy until she started frantically searching for a way to save her husband, whose infection was not responding to even the most powerful antibiotics. She had found a couple of papers on phage therapy shortly after making a promise to her husband that she would do everything she could do save him.
"I chose a day where I thought that he could hear me, and I asked him, basically, if he wanted to live or die," Strathdee said in an interview. "And when he squeezed my hand, I took that as 'okay, I'm not to keep him alive for my sake or his daughters' sake; this is what he wants.'"
From that point on, Strathdee would become intimately familiar with the promise—and the problems—of bacteriophage therapy.
A vacation ends with a superbug infection
Patterson, 67 at the time, acquired his infection after suffering a bout of gallstone pancreatitis during a vacation in Egypt in November 2015. Initially treated at a clinic in Luxor, his condition worsened to the point where he had to be medivacked to Frankfort, Germany, where he was found to have a large pancreatic pseudocyst that was infected with drug-resistant A baumannii, an opportunistic microbe that has been labeled a priority pathogen by the World Health Organization.
After suffering several severe sepsis episodes while in Germany, Patterson was flown back to the United States in December for treatment at UCSD Health. By this point his infection was resistant to several classes of antibiotics, including last-resort antibiotic therapies like carbapenems and colistin.
"Tom's Acinetobacter baumannii had something like over 40 resistance genes and acquired six more over a 3-week period," Strathdee said.
New antibiotics added to the regimen would work for a little while and Patterson's condition would stabilize, but then the infection would develop resistance to the new drugs. Things got very bad in late January, when one of the percutaneous catheters that had been inserted into his abdomen to drain the pseudocyst slipped and spilled the bacteria into his peritoneal cavity. From there, it began to spread throughout his body. Respiratory and renal failure ensued, and Patterson fell into a coma (see photo at left, courtesy of Steffanie Strathdee).
"It was basically a story of multi-organ system failure in the presence of an infection we couldn't get on top of because of multidrug-resistance," said Robert "Chip" Schooley, MD, who was chief of the infectious diseases division at UCSD School of Medicine and the lead physician on the case.
"From that moment onward, he was in and out of a coma and just started getting worse," said Strathdee. "I think everybody was thinking there'd be some sort of turnaround, but it was pretty clear that it was a downward trajectory, and so that's when I took matters into my own hands."
Soon after Strathdee started diving into the literature on bacteriophages, she received an email from a colleague at the University of California, San Francisco about a friend who had undergone phage therapy in Tblisi, Georgia for a superbug infection. Intrigued by the potential, she brought up the idea of phage therapy with Schooley, who initially thought the idea was premature but was willing to give it a try.
If Strathdee could find the phages that would specifically attack A baumannii, Schooley told her, he would file an Emergency Investigational New Drug (eIND) application with the Food and Drug Administration (FDA). Physicians can request use of an unapproved, investigational drug when the need is urgent and there are no other alternatives available.
With Patterson's condition worsening, Strathdee began emailing and calling phage researchers around the world to see if they might have phages that could be used to treat his infection. Her first response came in mid-February, from Ryland Young, PhD, director of Texas A&M's Center for Phage Technology.
It wasn't the first time he'd received such a request, said Young. He regularly receives requests for phages from desperate family members or friends of patients with life-threatening infections, and always turns them down, since phages aren't approved by the FDA and the request needs to come through a physician. Plus, said Young, "We're a research lab, not a clinical production lab, so that's the other side of it."
But Strathdee came to Young not only with an urgent need but also with an impressive understanding of the science and, more importantly, a doctor who was willing to give phage therapy a try. She made a compelling argument for Young to help her out.
"She was very motivated but also very knowledgeable," said Young.
Though Young was skeptical about whether he would able to help Patterson given the dire circumstances, he decided to give it a go. What he would need was an isolate of Patterson's A baumannii infection that he could test against his collection of phages.
Finding the right phages
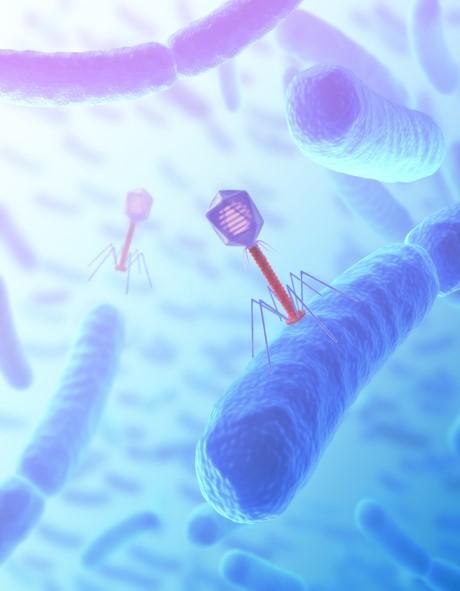
The concept of bacteriophage therapy isn't new. Microbiologists Frederick Twort and Felix d'Herelle each independently discovered the phenomenon that small viruses could selectively infect and kill specific bacteria without affecting other organisms more than a century ago. Despite the interest in using phage therapy to treat bacterial infections, the evidence for its effectiveness was inconsistent, and the American Medical Association "put the kibosh" on it, said Young, in a series of reports starting in 1934.
Once sulfa drugs and penicillin were discovered and the antibiotic era began, interest in phages waned. That interest, however, has been reignited in recent years as bacteria have become increasingly drug-resistant.
Bacteriophages aren't hard to find, either. They can be found anywhere bacteria exist—in soil, in the oceans, inside plants and animals, and in sewage water. In fact, they're particularly abundant in sewage water. But to treat a bacterial infection with phages, you have to find the phages that attack the specific pathogen causing the infection. That's where the real work begins. "Every bacterial pathogen has a different story in terms of phage," said Young.
And while Escherichia coli phages will kill all strains of that pathogen, A baumannii phages will kill only the strain with which they are matched. In other words, phages that kill one particular strain of A baumannii won't work against other strains of the bacterium.
Once Young and his colleagues at Texas A&M had gotten the necessary permissions and received one of Patterson's A baumannii isolates, they tested the 10 phages in their collection (which includes hundreds of phages) that they knew had activity against the pathogen. But none of those phages worked. "We knew within 1 day of getting the strain that we had to go on a good old-fashioned phage hunt," Young said.
Working around the clock, Young and his team then tested more than 100 environmental samples to find the right phages. Young also got in touch with other phage researchers around the world whom he knew had A baumannii phages in their collections. One company that sent phages was AmpliPhi Biosciences, a biotech company based in San Diego—just miles from the hospital where Patterson was being treated. About 5 days later, the Texas A&M team was able to find three phages from its environmental samples that had the ability to kill the strain of A baumannii that was attacking Patterson. A fourth phage, from AmpliPhi, was added to the mix.
Meanwhile, Schooley had also reached out to the Naval Medical Research Center (NMRC) in Silver Spring, Md. The NMRC has been developing phages as an alternative to antibiotics for several years, with a particular focus on A baumannii, which has earned the nickname "Iraqibacter" because of its association with infected combat wounds suffered by soldiers serving in Iraq. Within a few days of receiving an isolate, NMRC was able to come up with its own "cocktail" of four phages from sewage water that also wiped out Patterson's A baumannii strain.
Growing, purifying the phages
Finding the right phages, however, was just the first step. Both teams then had to grow enough phages to make a solution that could be used to treat the infection. To grow phages, you expose them to the strain of bacteria that they are active against in a petri dish. Once the phages latch onto a receptor on the bacterium, they insert their DNA inside the host cell, where it replicates and creates more phages. The newly created phages then break down the cell membrane and spill forth and diffuse outward, ready to attack more bacteria and create more progeny. The cleared zones of bacteria are called plaques.
But that process creates a problem, Young explains, especially with gram-negative bacteria. That's because the fluid containing the phages also contains the debris of hundreds of millions of bacterial cells, each of which is coated with endotoxins that could induce toxic shock when injected into a patient. "So you're starting off with something that's potentially useful, but it's contaminated with the worst possible contamination," Young said.
Since the FDA would not allow the phage cocktails to be used until the endotoxins levels were low enough that the treatment could be attempted safely, the two teams then had to purify the phages, a laborious and painstaking process that involves separating the phages from the endotoxins through filtration and high-speed centrifugation. The purified phages are then added to a saline solution. Meanwhile, the clock was ticking.
"The biggest amount of time was the endotoxin purification, which is just the biggest pain," Strathdee said. "The whole endotoxin issue probably delayed things by a week."
"We had a graduate student and couple of technicians who basically worked 24/7," said Young. "But when you're dealing with a patient that is trying to get through one more day, it's very easy to say 'I guess I'll go back in and spin down those phages and purify them again.'
"It was very motivating, and some ways exhilarating, but it was grueling."
"If it had been another week in getting the phages prepared, we probably would have lost the patient," said Schooley. "The timing was extremely close."
Phage therapy begins
By Mar 15, the phages from Texas A&M were purified and ready to go, and Schooley received approval from the FDA to go forward with the treatment. It was the same day that Strathdee was asked to sign a consent form for dialysis for her husband's failing kidneys.
One problem, though, was that there were no clear instructions on what kind of dose to use and how often to administer the therapy. Schooley and his colleagues basically had to make up the regimen as they went along. "This was a seat-of-the-pants thing, for sure," said Strathdee.
The physicians began by inserting the phage cocktail through the catheters into Patterson's abdominal cavities—the site of the initial infection—to make sure he could tolerate it. Over the next 36 hours, Patterson's condition stopped deteriorating, "but he certainly didn't seem to be getting better," said Schooley. Then, on Mar 17, they started delivering the Navy's phage cocktail intravenously to go after the bacteria that had spread to other parts of his body. That's when they started to see a clear response in his clinical features.
"And after that, 48 hours later, he was clearly much better," Schooley said.
Patterson emerged from his coma and was able to communicate with his family for the first time in nearly 2 months. And the phage therapy appeared to have no adverse effects.
"It was really remarkable," said Strathdee.
Patterson wasn't out of danger yet, though. While his infection was now susceptible to the antibiotic minocycline, his condition was still tenuous as he dealt with issues that 67-year-old patients in intensive care units frequently face. And after several weeks of phage therapy, in vitro testing of isolates indicated that the A baumannii infection was becoming less susceptible to the phage cocktails.
At that point, Schooley sent a new isolate to the NMRC, which was developing new methods to quickly identify and purify phages and wanted to test its approach. Within 3 days of receiving the isolate, the Naval researchers found another phage from sewage water that inhibited growth of the strain, combined it with one of the phages from their initial phage cocktail, and created a third phage cocktail that was administered in late April. Over the following weeks, Patterson's condition continued to improve.
On Aug 12, 245 days after he entered the hospital, Tom Patterson, a hundred pounds lighter and still physically and mentally weak, finally went home.
The future of bacteriophage therapy
So did bacteriophages save Patterson's life? As is often the case in medicine, there's no simple answer to that question.
"I'd be the last one to say, dogmatically, that if it hadn't been for the phage he'd be dead, because there are a lot of things going on," said Schooley.
That conclusion is reflected in a paper published online on Aug 14 in Antimicrobial Agents and Chemotherapy. "As with any uncontrolled clinical observation, there are a number of important caveats; primarily, we cannot exclude the possibility that the reversal of his clinical deterioration was unrelated to the phage therapy," Schooley and his co-authors wrote. "However, after an inexorably downhill clinical course over the prior three months to the point that discussion about clinical futility had been initiated, a clear turning point was observed within 48 hours of starting intravenous bacteriophage therapy."
The paper also notes that it appears that the phages were working synergistically with the minocycline against the infection. "We showed in the laboratory that there was added activity between minocycline and the phage that we used," Schooley explained. "I think there's a natural synergy, in a number of ways, in which phages can make bacteria either more sensitive to antibiotics, or constrain the ability of the organism to evolve to become resistant to antibiotics."
In addition, Schooley notes that as the A baumannii mutated to become more resistant to the initial phage cocktails, it also became less invasive.
Young thinks that it's possible that the mutation caused by the selection pressure of the phages may have made the bacteria more permeable and therefore more susceptible to antibiotics. But he also suggests that the phages' ability to swiftly and thoroughly kill the A baumannii likely reduced the bacterial load to the point where Patterson's antibodies could kick in and help fight the infection. "Your guess is as good as mine," he said.
Patterson and Strathdee are little less cautious in their assessment.
"As a skeptical scientist who has written and reviewed many papers, I'm someone who always looks for scientific evidence," said Patterson. "And even if you are skeptical about this finding, what it provides is evidence-based hope that we may finally have some new avenue to battle superbugs.
"I'm hopeful that my experience is really going to move the field forward," he added. Patterson also acknowledges that he was very fortunate to have a spouse who was a powerful advocate and to be treated at a university hospital with top-notch clinicians and caregivers.
"I don't think there's any doubt that the phages did something, and the synergy with the antibiotics probably also played a role," said Strathdee. "But that's why we need clinical trials."
Schooley agrees.
"I think there are a number of places where phages might turn out to be extremely useful, and what we need to do is organize structured, well-designed, well-conducted clinical trials, just like you would with any new therapeutic, to figure it out," he said. Both he and Strathdee believe that phage therapy's greatest potential may be as an antibiotic adjuvant.
"Even if phages by themselves aren't important, the fact that they could make antibiotics that aren't working work again is a big deal," said Strathdee.
For his part, Young would prefer not to be in another situation where his lab—or any phage researchers—are desperately trying to find and purify bacteriophages for patients who have run out of options. "It's just not sustainable," he said.
With FDA approval of phage therapy likely a long way off, he thinks research labs and hospitals should at least be better prepared for emergency requests by having libraries of fully characterized and purified phages that they know will work against different types and strains of bacteria. And preferably, he would like to see collections of phages that work on different bacterial cell receptors, which would reduce the ability of bacteria to develop resistance to phage cocktails. That would at least reduce some of the workload and time.
The NMRC is on the same page. "Our goal with the Navy phage therapeutic program is to establish a phage library that will be large and comprehensive enough so that previously isolated, well characterized phages will be in hand and ready to use," an NMRC spokesperson said.
Strathdee would also like to see phage therapy be more than a last-ditch effort. "That's the dilemma that we're in right now," she said. "You have to wait until someone's at death's door before they're even eligible to get an eIND."
One possibility, she suggests, would be for the FDA to loosen its current restrictions to allow phage therapy for people who aren't in a life-threatening situation but have a multidrug-resistant infection and are willing to take the risk.
No matter what, Strathdee and Patterson, who are co-writing a book about their experience titled, Perfect Predator: An Epidemiologist's Journey to Save Her Husband from a Deadly Superbug, say they will continue to advocate for phage therapy as one potential solution to antibiotic resistance problem. "We think there's a global imperative here to consider something that's been right under our noses," Strathdee said. "It really could be a solution for the antimicrobial resistance crisis if it's shown to be efficacious."
See also:
Aug 14 Antimicrob Agents Chemother study
Oct 17 TEDxNashville: "How sewage saved my husband's life from a superbug"