A new ultra-rapid, phenotype-based antimicrobial susceptibility testing (AST) method eliminates the need for conventional blood culture in patients with suspected sepsis, potentially speeding antibiotic prescription by upwards of 40 to 60 hours, scientists reported yesterday in Nature.
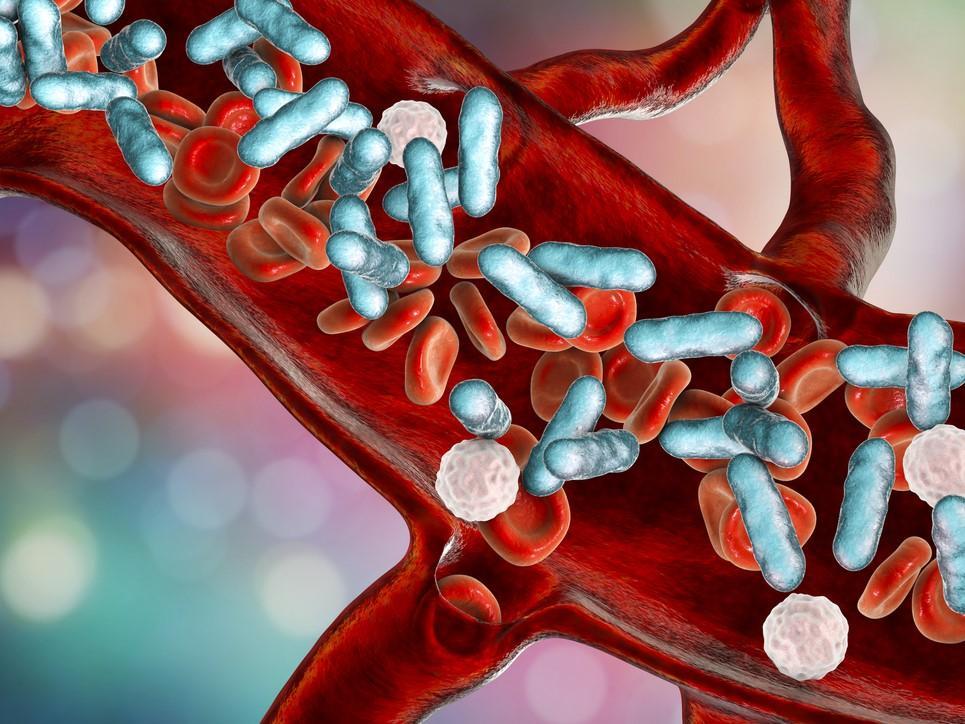
Researchers at Seoul National University in South Korea describe the addition of magnetic nanoparticles into whole blood. "The principle is simple," senior author Sunghoon Kwon, PhD, of Seoul National University, said in a Nature podcast. "We have a magnetic nanoparticle. The surface of the magnetic nanoparticle we coat in a peptide that can capture the bacteria."
The need for timely treatment
The test, the researchers said, allows the selective isolation of microbial pathogens for expedited culture with pure media to evaluate their drug susceptibility with the use of a low-inoculum, phenotypic imaging-based AST chip.
"Treatment assessment and patient outcome for sepsis depend predominantly on the timely administration of appropriate antibiotics," the study authors noted. "However, the clinical protocols used to stratify and select patient-specific optimal therapy are extremely slow," due to the 2- to 3-day blood culture procedure.
"The microbial load in patient blood is extremely low, ranging between 1 and 100 colony-forming units (CFU) ml−1 and is vastly outnumbered by blood cells," they explained. "Due to this disparity, prior steps—including blood culture (BC) to amplify the number of pathogens followed by pure culture to subculture purified colonies of isolates—have been essential for subsequent pathogen species identification (ID) and AST."
100% match in species identification
To determine pathogen enrichment performance, the researchers spiked five of the most common infecting strain cell lines into 5 milliliters of phosphate-buffered saline (PBS) or blood with different bacterial loads.
"The entire procedure was completed within 1 h [hour] following nanoparticle injection, pathogen binding, magnetic separation and resuspension into 1 ml of PBS or fresh cation-adjusted Mueller–Hinton broth (MHB) culture medium," they wrote.
With the optimized protocol, capture efficiency of 96.2% and 91.5% was confirmed for Escherichia coli and Staphylococcus aureus, respectively. Using pure media in which the blood components were removed enhanced pathogen growth 9.8-fold and 19.0-fold over standard culture.
With the potential to guide clinicians towards timely administration of optimal therapy, thereby saving many lives, our platform can also help to de-escalate the spread of antimicrobial resistance and sustain the lifespan of existing antibiotics.
When the team evaluated the new test performance in 190 hospitalized patients with suspected infection, they achieved a 100% match in species identification. Six clinical isolates from eight infected patients that were retrospectively tested for AST had an overall categorical agreement of 94.9% and an average theoretical turnaround time from initial blood processing of 13 hours, plus or minus 2.5 hours.
Could help slow spread of antimicrobial resistance
"With the potential to guide clinicians towards timely administration of optimal therapy, thereby saving many lives, our platform can also help to de-escalate the spread of antimicrobial resistance and sustain the lifespan of existing antibiotics," the researchers concluded, saying that future validation with a more diverse patient cohort is needed.
Because traditional blood culture is time-consuming, clinicians must initiate empirical, broad-spectrum antibiotics, the researchers said. "This implies that often inadequate prescriptions made during the initial treatment phase might jeopardize patient survival until a valid AST result is available," they wrote. "Among antimicrobial drugs prescribed to human patients, 14–78% were estimated to be unnecessary or ineffective."
While the initial use of these antibiotics is unavoidable, the authors said that AST results should ideally be ready as soon as the second dose of the prescription.
Recent studies, they added, have shown that the risk of death, length of hospital stay, and healthcare costs could be improved by shorter TATs. "Therefore, the development of new strategies to substantially reduce total TAT for AST is critical," they wrote.