A new analysis of the burden of antimicrobial resistance (AMR) in Europe estimates that drug-resistant bacteria were linked to more than half a million deaths in the region in 2019.
The study, published yesterday in The Lancet Public Health, found that, across the 53 countries of the World Health Organization's (WHO's) European Region, 541,000 deaths were associated with bacterial AMR, and 133,000 deaths were directly attributable to drug-resistant pathogens. The highest mortality rates both attributable to and associated with AMR were in Eastern Europe, followed by Central Europe.
The vast majority of AMR deaths were caused by seven bacterial pathogens, with methicillin-resistant Staphylococcus aureus (MRSA) and aminopenicillin-resistant Escherichia coli among the primary culprits.
The study authors say the analysis provides the most detailed, comprehensive assessment to date of the AMR burden in Europe.
"The high levels of resistance for several important bacterial pathogens and pathogen–drug combinations, together with the high mortality rates associated with these pathogens, show that AMR is a serious threat to public health in the WHO European region," they wrote.
Attributable and associated deaths
The study, conducted by an international team of scientists and led by researchers with the University of Washington's Institute for Health Metrics and Evaluation, used data from a variety of sources to estimate, through statistical modeling, deaths and disability-adjusted life-years (DALYs) attributable to and associated with 23 bacterial pathogens and 88 drug-pathogens in the WHO European Region in 2019.
Overall, 471 million individual records or bacterial isolates were obtained from sources such as the European Antimicrobial Resistance Surveillance Network, the Central Asian and European Surveillance of Antimicrobial Resistance Network, and the WHO's Global Antimicrobial Resistance Surveillance System (GLASS).
The methodology in the study was similar to the approach used in the Global Research on Antimicrobial Resistance (GRAM) report published earlier this year, which estimated that 1.27 million deaths globally were directly attributable to AMR in 2019 (out of 4.95 million that were associated with drug-resistant pathogens). The authors say this study extends those results while providing more granular and country-specific estimates within Europe.
As in the GRAM report, the researchers calculated the AMR burden (deaths and DALYs) using an approach based on two counterfactual scenarios. To estimate deaths directly attributable to resistant bacteria, they considered a scenario in which those infections were replaced by antibiotic-susceptible infections. To estimate associated deaths, they considered a scenario in which resistant infections were replaced by no infection.
Of the estimated 133,000 attributable deaths (95% uncertainty interval [UI], 90,100 to 188,000) and 541,000 associated deaths (95% UI, 370,000 to 763,000), the largest fatal burden from AMR came from bloodstream infections, with 47,200 attributable deaths and 195,00 associated deaths linked to any resistant drug-pathogen combination. Other leading causes of deaths from any resistant drug-pathogen combinations were intra-abdominal infections (31,200 attributable and 127,000 associated deaths) and respiratory infections (28,500 attributable and 120,000 associated deaths).
Seven leading bacterial pathogens were responsible for 112,784 attributable deaths and 457,591 associated deaths: E coli, S aureus, Klebsiella pneumoniae, Pseudomonas aeruginosa, Enterococcus faecium, Streptococcus pneumoniae, and Acinetobacter baumannii.
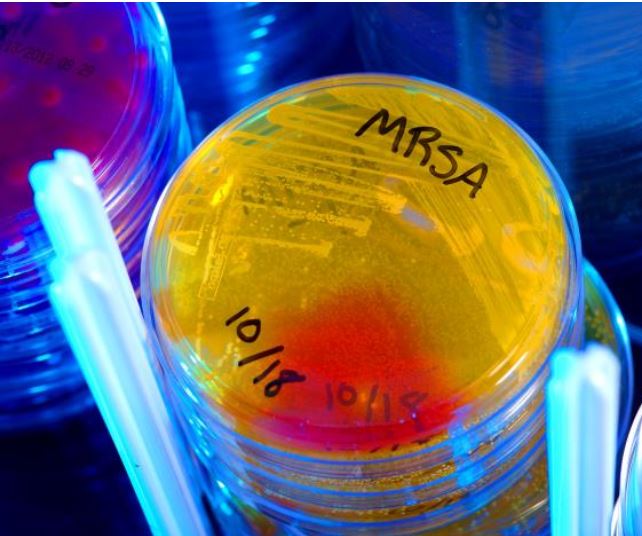 MRSA was the leading drug-pathogen combination for deaths attributable to AMR in 27 countries (51% of the region), while aminopenicillin-resistant E coli was the leading drug-pathogen combination for associated deaths in 47 countries (89% of the region). A similar distribution was observed with DALYs for pathogen-drug combinations.
MRSA was the leading drug-pathogen combination for deaths attributable to AMR in 27 countries (51% of the region), while aminopenicillin-resistant E coli was the leading drug-pathogen combination for associated deaths in 47 countries (89% of the region). A similar distribution was observed with DALYs for pathogen-drug combinations.
The estimated mortality rates per 100,000 population observed in Eastern Europe (19.9/100,000 attributable and 74.0/100,000 associated) and Central Europe (16.6/100,000 attributable and 68.0/100,000 associated) were considerably higher than those in Western Europe (11.7/100,000 attributable and 52.5/100,000 associated). Accounting for age-standardized mortality rates per 100,000, the countries most affected by AMR were concentrated in Central Asia (which is considered by the WHO to be part of the European Region).
The analysis also found that countries in the region with developed, approved, financed, and implemented national AMR action plans were in the lowest 50th percentile of age-standardized mortality rates, both for attributable and associated deaths. Nations with lower socio-demographic index (SDI) scores—a measurement of overall development—had a larger AMR mortality burden.
In addition, a positive correlation between crude AMR mortality rates and antimicrobial use was observed, with the strongest relationship seen in Western and Central Europe.
AMR mitigation strategies needed
When compared with the estimates from the GRAM report, the WHO European region—which makes up approximately 12% of the world's population—accounts for 10.5% of the estimated 1.27 million global deaths attributable to AMR, and 10.9% of the estimated 4.95 million associated deaths.
In an accompanying commentary, infectious disease experts from the Geneva University Hospitals and Faculty of Medicine say the findings illustrate the substantial adverse health impact that AMR-related infections have throughout Europe. They add that future AMR mitigation strategies in the region will require developing and maintaining high-quality AMR surveillance networks to advance knowledge of the true burden of AMR, funding research to evaluate the burden of specific resistant-pathogen combinations and develop pathogen-specific interventions, and quantifying the economic impact and indirect costs attributable to AMR.
"All these elements can bridge knowledge gaps and pave the way towards an exit strategy from this silent pandemic," Nasreen Hassoun-Kheir, MD, and Stephan Harbarth, MD, wrote.
They also say the findings should encourage clinicians and policymakers throughout Europe to endorse and implement country-specific AMR control plans, with a parallel focus on implementing the best infection control and antibiotic stewardship programs in healthcare settings.

























