The results of a randomized clinical trial conducted in the United Kingdom suggest a non-antibiotic antiseptic treatment may be as good as antibiotics for preventing recurrent urinary tract infection (UTI), researchers reported yesterday in The BMJ.
The drug, methenamine hippurate, has previously been evaluated in systematic reviews for the prevention of recurrent UTI, which occurs in roughly one in four women who have a UTI episode, but the results of those reviews have been inconclusive. This is the largest randomized trial yet to assess its efficacy compared with antibiotics—the current standard treatment.
The results showed that while women who received prophylactic treatment with methenamine hippurate had a higher rate of UTI episodes than those treated with prophylactic antibiotics, the absolute difference has limited clinical significance.
The study authors say the findings could support a change in practice that may help patients with recurrent UTI avoid long-term antibiotic use and thus potentially help combat antibiotic resistance.
Non-inferiority margin met
In the ALTAR trial (alternative to prophylactic antibiotics for the treatment of recurrent urinary tract infections in women), a team of investigators from the United Kingdom recruited adult women who had at least three UTI episodes in the previous 12 months from urology and urogynecology centers.
Over a span of 12 months, participants were randomly assigned 1:1 to receive either twice-daily oral doses of methenamine hippurate or daily doses of antibiotics (nitrofurantoin, trimethoprim, or cefalexin), with a 6-month follow-up period.
Participants, clinicians, and research staff were not masked in the trial, and participants were allowed to switch between treatment strategies, though the need to adhere to the allocated intervention was emphasized by investigators.
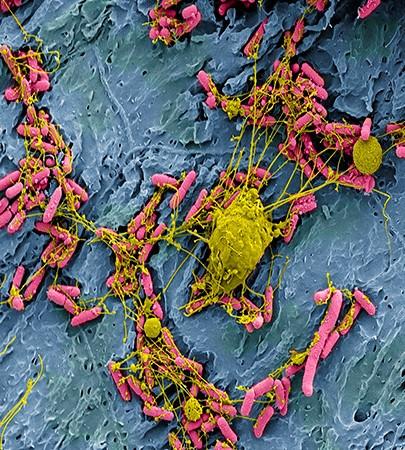
The primary clinical outcome was the incidence of self-reported symptomatic, antibiotic-treated UTIs over the 12-month treatment period. Secondary outcomes included incidence of UTIs during the 6-month follow-up period, total antibiotic use, and antibiotic-resistance profiles in Escherichia coli isolated from urine and perineal swabs. The non-inferiority margin was a difference of one UTI episode per year.
A total of 240 patients were recruited for the trial, and 205 were included in the modified intention-to-treat analysis—102 in the antibiotic arm and 103 in the methenamine Hippurate arm.
Over the 12-month treatment period, the incidence of symptomatic UTI was 0.89 episodes per person year (95% confidence interval [CI], 0.65 to 1.12) in the antibiotic arm and 1.38 (95% CI, 1.05 to 1.72) in the methenamine hippurate arm, for an absolute difference of 0.49 (90% CI, 0.15 to 0.84). Secondary analyses of the primary outcome showed consistent results that were within the non-inferiority margin.
"The observed numerical difference in clinically diagnosed UTI between the two trial arms, which favoured antibiotic prophylaxis, was small and did not exceed the predefined non-inferiority margin of one episode per person year," the study authors wrote.
In the 6-month follow-up period, the UTI incidence rate was 1.19 (95% CI, 0.86 to 1.52) in the antibiotic arm and 1.72 (95% CI, 1.27 to 2.18) in the methenamine hippurate arm, for an absolute difference of 0.53.
Therapeutic antibiotics for UTI were received by 43% of participants in the antibiotic arm and 56% in the methenamine hippurate arm over the 12-month treatment period. But overall antibiotic use among women who received prophylactic methenamine hippurate was lower.
The proportion of participants demonstrating resistance to at least one antibiotic in E coli isolated from perineal swabs was higher in the antibiotic arm (46 of 64, 72%) than in the methenamine hippurate arm (39/70, 56%), and results from urine cultures showed higher rates of resistance in E coli to trimethoprim, co-trimethoxazole, and cephalosporins. At month 18, however, multidrug resistance in E coli was higher in the methenamine group (20% vs 5%).
On average, treatment satisfaction was high in both groups, and adverse events were low and comparable; 24% were reported in the antibiotic arm and 28% in those who received methenamine hippurate.
Avoiding antibiotic consumption
"The information provided by this trial will allow clinicians and patients to undertake a shared decision-making process relating to UTI preventive treatments," the authors wrote. "The study showed a small numerical difference in UTI incidence between the daily antibiotics and methenamine hippurate groups, but the potential trade-off includes the avoidance of antibiotic consumption, which is closely associated with antimicrobial resistance development."
In a linked commentary that accompanies the study, researchers from the Institute for Evidence Based Healthcare at Australia's Bond University say that, given the frustration voiced by women who experience recurrent UTI, and the concerns about frequent antibiotic use and its related consequences (namely antibiotic resistance and adverse events), identifying strategies to minimize antibiotic use is important for both individuals and the community.
They note that while the trial has limitations, including the lack of blinding and comparison with several antibiotics, they agree the findings could help inform conversations between clinicians and patients that take into account the benefits and harms of antibiotic use and each patient's values and preferences.
"Although the results need cautious interpretation, they align with others, and this new research increases the confidence with which methenamine hippurate can be offered as an option to women needing prophylaxis against recurrent urinary tract infection," they wrote.