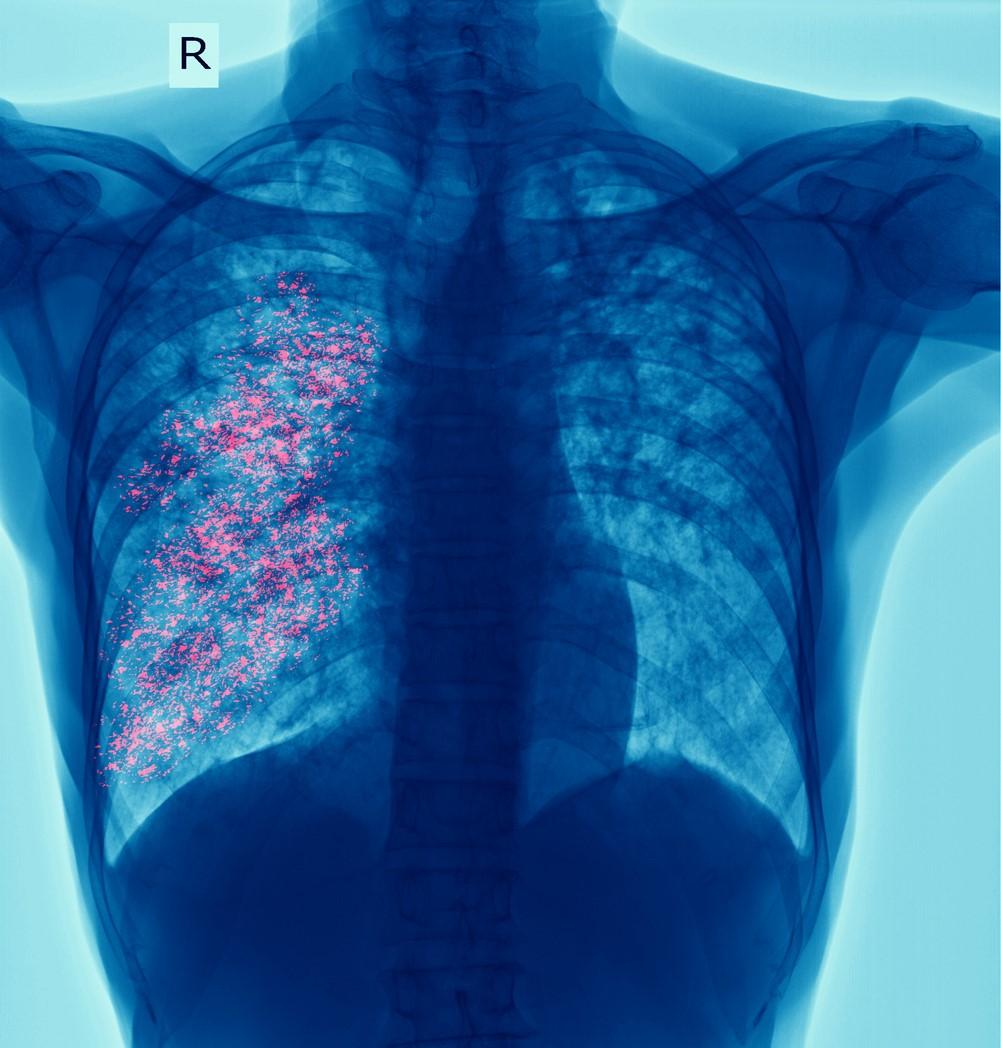
A new study by researchers with the Centers for Disease Control and Prevention and Harvard T.H. Chan School of Public Health has found significant and persistent racial disparities in tuberculosis (TB) incidence among US-born residents. The findings were published yesterday in the Annals of Internal Medicine.
While racial disparities have long been present in US TB incidence, because most cases occur among people from racial and ethnic minority groups born outside the United States, few studies have examined racial disparities in TB incidence specifically among the US-born population.
To do so, the researchers analyzed data from the National Tuberculosis Surveillance System on US-born patients with reported TB disease from 2011 through 2021, comparing TB incidence rates, incidence rate differences, and incidence rate ratios among different racial and ethnic minority groups. They stratified the results by sex, age-group, and whether TB disease was attributed to recent transmission.
More than 18,000 excess TB cases attributed to disparities
Among the 31,938 TB cases in US-born patients analyzed, researchers found substantially higher incidence among racial/ethnic minority populations. Compared with non-Hispanic Whites, TB incidence rate ratios were 4.4 times higher for Hispanics, 6.6 times higher for Asians, 6.8 times higher for Blacks, and 14.2 times higher for American Indian/Alaska Natives. Within each racial/ethnic population, absolute disparities in incidence rates were generally greater for males than females, while relative disparities were greater for females, younger people, and those who had TB attributed to recent transmission.
Over the course of the study period, the researchers estimate there were 6,950 excess TB cases attributable to racial/ethnic disparities among women, 11,130 among men, and 18,080 total.
The study authors say addressing these disparities is crucial for achieving health equity goals and accelerating progress toward population-level TB elimination. "Ongoing measurement of disparities will be needed to track progress toward these targets," they wrote.
In an accompanying editorial, infectious disease experts from Emory University Rollins School of Public Health suggest the data could be used to inform targeted efforts by state and local TB programs to focus on early detection and care among high-risk groups.

 A California Department of Public Health
A California Department of Public Health 











