An increase in uptake of routine childhood vaccines among US children over 15 years was associated with a decrease in antibiotic prescriptions and antibiotic-treated sinus infections, according to an ecological study published today in Antimicrobial Stewardship & Healthcare Epidemiology.
Using de-identified commercial claims data, researchers from Merck and Analysis Group Inc. analyzed uptake of four pediatric vaccines recommended by the Centers for Disease Control and Prevention for children aged 5 years and younger: the 7- or 13-valent pneumococcal conjugate vaccine, Haemophilus influenzae type b (Hib) vaccine, diphtheria-tetanus-acellular pertussis (DTaP) vaccine, and influenza vaccine. Vaccination status was assessed annually from 2000 through 2019, and children were categorized based on receipt of all 4 vaccines, 1 to 3 vaccines, or no vaccines.
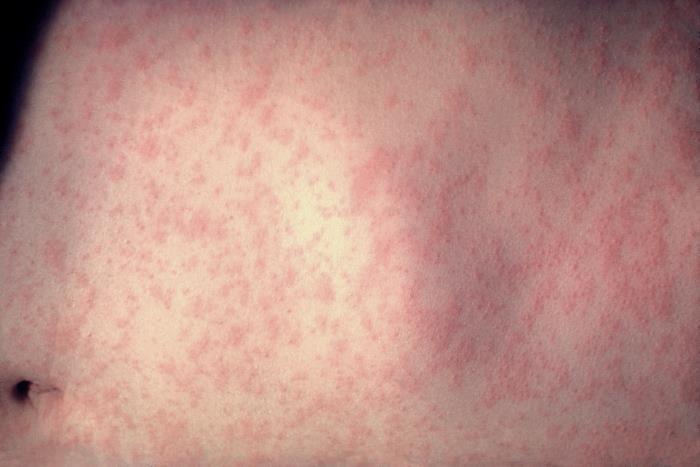
The primary outcomes were antibiotic prescriptions for any reasons and five respiratory tract infections that commonly result in antibiotic prescriptions: otitis media (ear infection), pharyngitis, pneumonia, sinusitis, and viral respiratory infections.
Antibiotic prescriptions nearly cut in half
Data from 6.7 million children showed that vaccine uptake more than doubled over the study period, from 32.5% of children receiving one dose of the four vaccines in 2004 (the first year all 4 vaccines were recommended) to 66.8% in 2019. The proportion of unvaccinated children fell from 8.4% in 2004 to 2.5% in 2019. At the same time, overall antibiotic prescriptions decreased from 1.89 to 1.01 per person-year from 2000 through 2019, and the rate of overall antibiotic prescriptions decreased by 46.6%. The greatest reduction in comparison to 2000 was seen in macrolides (73.3%) and broad-spectrum antibiotics (57%).
Antibiotic-treated respiratory tract infections declined from 2.43 to 1.61 episodes per person-year, with the largest decreases in sinusitis (64.7%) and pharyngitis (39.8%). The incidence of overall antibiotic-treated respiratory tract infections decreased by 33.8% in 2019 compared with 2000.
"Although causality cannot be inferred due to the ecological study design, the observed trends are consistent with the notion that reducing vaccine-preventable diseases may decrease antibiotic use," the study authors wrote. "While various factors besides vaccination may also play a role, future prospective cohort studies using longitudinal patient-level data are warranted to validate this association."