 An analysis of stool samples from patients in Mozambique, nearly half of whom had HIV, found high rates of antibiotic resistance in diarrheal pathogens, researchers reported late last week in BMC Infectious Diseases.
An analysis of stool samples from patients in Mozambique, nearly half of whom had HIV, found high rates of antibiotic resistance in diarrheal pathogens, researchers reported late last week in BMC Infectious Diseases.
In the study, researchers from Mozambique and the United States conducted antibiotic susceptibility testing on 157 stool isolates recovered from 129 patients at two health centers, including 68 HIV infected and 61 uninfected individuals. The isolates, which consisted of 99 Salmonella, 45 Shigella, and 13 Campylobacter strains, were tested against six antibiotics on Mozambique's national essential medicines list.
All isolates drug-resistant
All isolates were resistant to at least one antibiotic, with the vast majority of Salmonella and Shigella isolates resistant to trimethoprim-sulfamethoxazole (89.9% and 86.6%, respectively). In addition, most Salmonella isolates were resistant to erythromycin (88.9%) and tetracycline (76.8%), most Shigella isolates were resistant to tetracycline (68.9%), and most Campylobacter isolates were resistant to erythromycin, azithromycin, and tetracycline (92.3% for all three antibiotics). Multidrug resistance was observed in 79.8% of Salmonella, 76.9% of Campylobacter, and 57.8% of Shigella isolates.
Drug susceptibility profiles for Salmonella and Campylobacter were similar in HIV-infected and uninfected patients, but Shigella isolates from uninfected patients were significantly more likely to be resistant to erythromycin or azithromycin or exhibit multidrug resistance.
The high prevalence of antibiotic resistance findings in this study is likely due to multiple factors.
The study authors say the high rate of resistance to trimethoprim-sulfamethoxazole is particularly concerning, since it is often the treatment of choice for patients with diarrhea and is used as prophylaxis for opportunistic infections in HIV patients.
"Overall, the high prevalence of antibiotic resistance findings in this study is likely due to multiple factors, including unrestricted and inappropriate use of antibiotics through self-medication, the sale of antibiotics in informal markets, cross-contamination through environmental and food sources, and the use of antibiotics in animal husbandry without proper guidance from healthcare professionals," the study authors wrote. "Our results highlight the critical need for implementing measures to promote responsible antibiotic use in both human and animal populations."
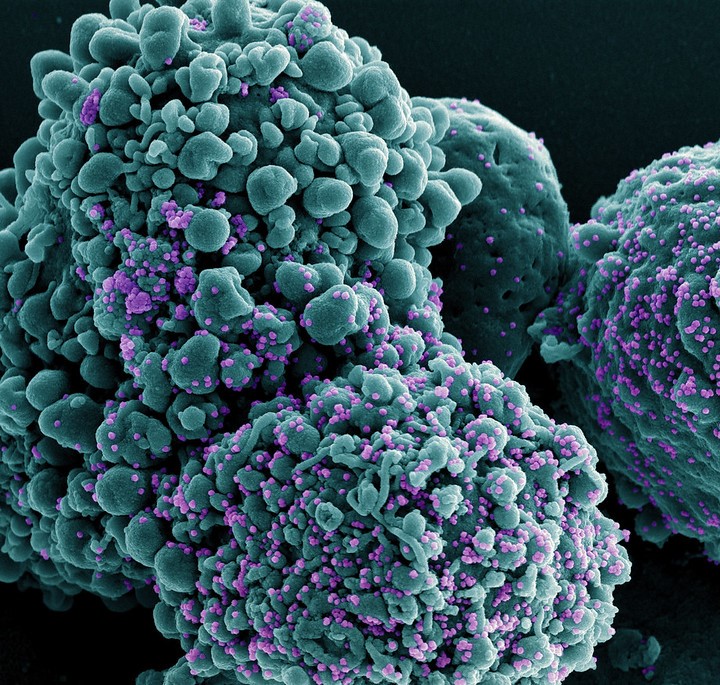
 Shielding, a public health strategy used across the United Kingdom in the early months of the pandemic, aimed to keep the most vulnerable citizens protected from the novel coronavirus at home and away from public-facing jobs and schools. But a new study of Welsh citizens published in the
Shielding, a public health strategy used across the United Kingdom in the early months of the pandemic, aimed to keep the most vulnerable citizens protected from the novel coronavirus at home and away from public-facing jobs and schools. But a new study of Welsh citizens published in the 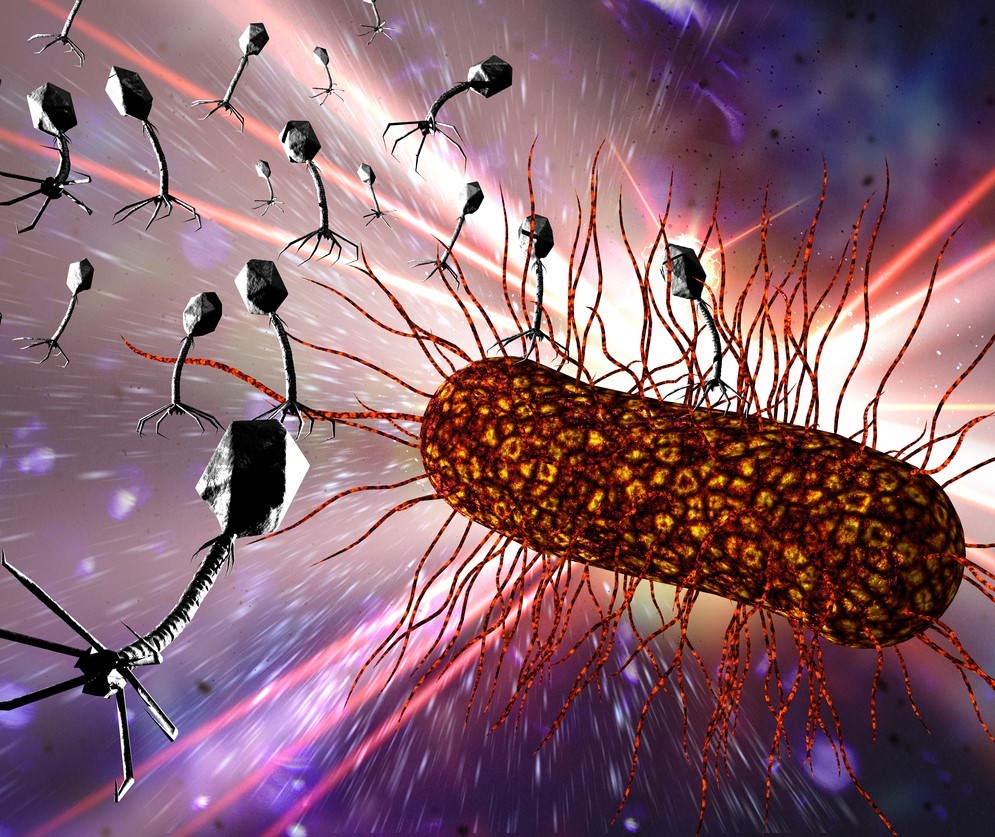 Researchers with the Israeli Phage Therapy Center (IPTC)
Researchers with the Israeli Phage Therapy Center (IPTC) 














