A study of the leading bacterial causes of travelers’ diarrhea (TD) found wide regional variations in nonsusceptibility to the two classes of antibiotics used for treatment, an international team of researchers reported last week in JAMA Network Open.
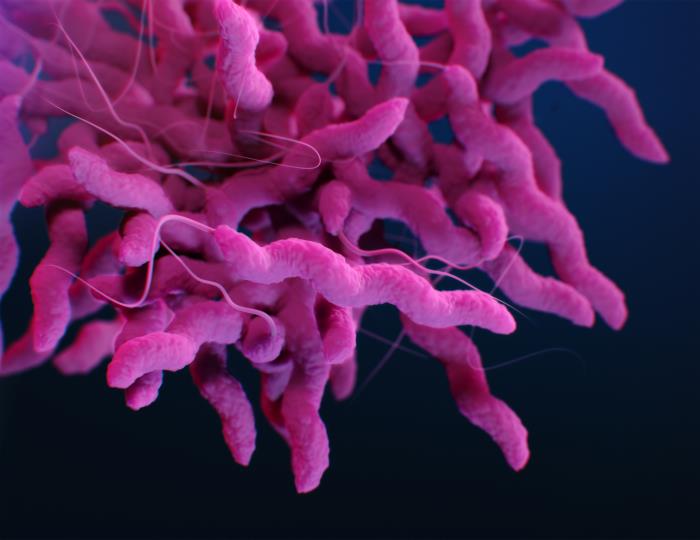
Using data from GeoSentinel, a worldwide network of tropical medicine centers located on six continents, the researchers conducted a retrospective cross-sectional analysis of antimicrobial susceptibility data for four major pathogens causing TD, reported from April 14, 2015 to December 19, 2022. The main outcomes were demographics, clinical characteristics, and antimicrobial susceptibility profiles of patients with culture-confirmed Campylobacter, Shigella, nontyphoidal Salmonella, and diarrheagenic Escherichia coli infections.
Current guidelines recommend fluoroquinolones or azithromycin (a macrolide antibiotic) for the management of moderate-to-severe acute TD. The study authors note that rates of resistance among isolates infecting international travelers have been limited to single-center studies.
Critical information for empiric treatment
Among pathogens isolated from 859 cases (median age, 30; 51% male) of TD from 103 countries, nonsusceptibility to fluoroquinolones was 75% for Campylobacter, 32% for nontyphoidal Salmonella, 22% for Shigella, and 18% for diarrheagenic E coli species. Among Campylobacter species, the highest proportion of nonsusceptibility to fluoroquinolones was observed in travelers to South Central Asia (88%), Southeast Asia (80%), and sub-Saharan Africa (60%).
Nonsusceptibility to macrolides was 12% for Campylobacter, 35% for Shigella, and 16% for Salmonella; 78% of Shigella isolates from South America and 24% of Campylobacter isolates from South Central Asia were nonsusceptible to macrolides. Twenty-six cases of Campylobacter infection were nonsusceptible to both fluoroquinolones and macrolides.
“Our findings have the potential to provide critical information for both the selection of standby empiric antibiotics for self-management of TD, and the empiric treatment of acute diarrhea in travelers, by travel medicine and primary care health care practitioners,” the authors wrote. “Our study findings also demonstrate the importance of surveillance of culture and susceptibility testing in TD in order to identify geographic patterns of resistance.”
















