If drugs and medical treatments are in short supply during a pandemic, a new model shows how machine learning can help decide how to distribute medicines and reduce hospitalizations by up to 27%.
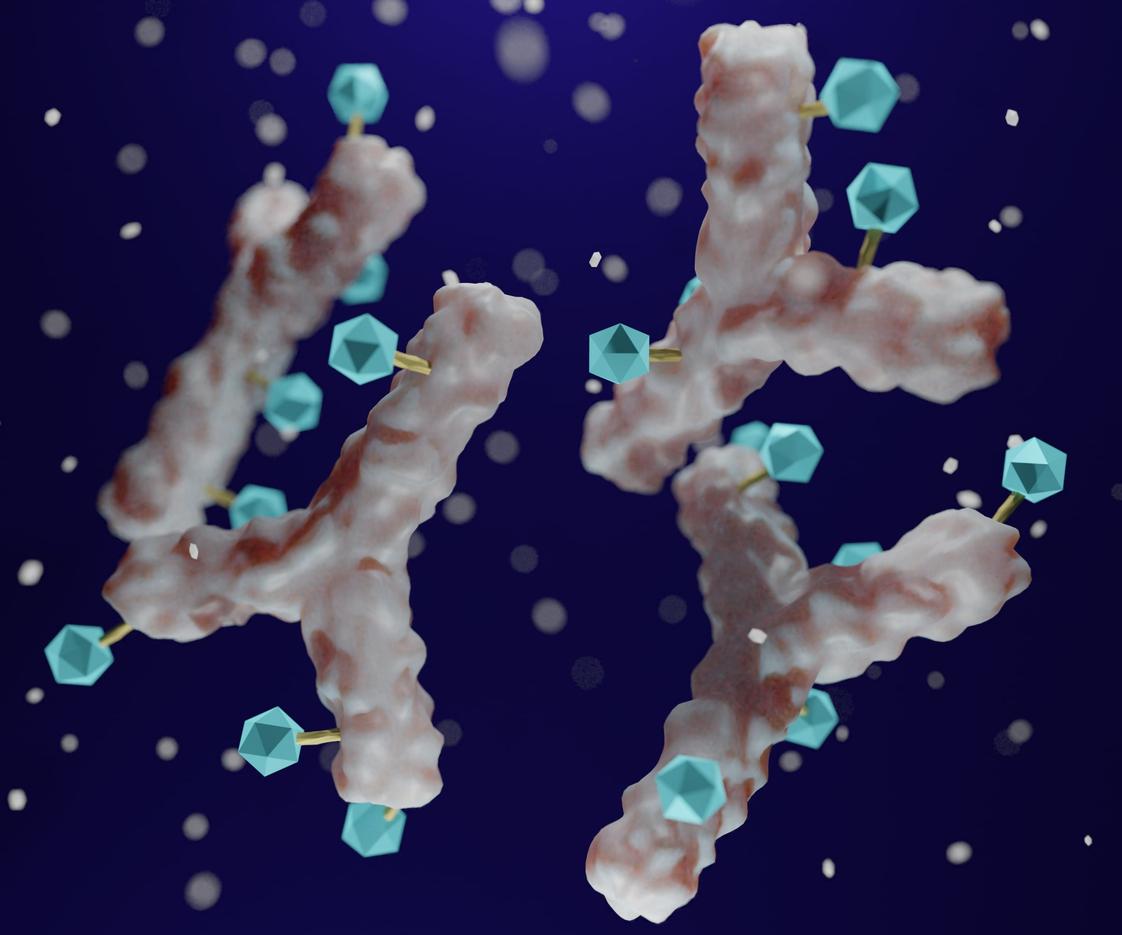
The study appears in JAMA Health Forum. The authors of the study explain that during the COVID-19 pandemic, many patients received treatment with monoclonal antibodies (mAbs) on a first-come, first-served basis or were treated based on individual health histories.
"But these methods often don't address the complex interactions that can occur in patients when taking medications to determine expected clinical effectiveness and may overlook patients who would benefit the most from treatment," said senior author Adit Ginde, MD, of the University of Colorado Anschutz Medical Campus in a press release from the university.
To create the model, authors used electronic health record data from more than 15, 000 patients with COVID-19 seen in a large healthcare system from October 1 to December 11, 2021, for the training cohort and data from June 1 to October 1, 2021, for the test cohort.
Policy learning tree considered vaccinations status, obesity
Instead of just targeting patients who are at greatest risk for hospitalization, the model, called a policy learning tree (PLT), instead considered both at-risk patients and those who would benefit most from treatments.
"To develop a PLT-based regression model, we used a forward model selection process using the top 5 important variables in PLTs (aged 65 years or older; fully vaccinated; aged 45 to 64 years; obesity; and cardiovascular disease)," the authors said.
They estimated the expected overall hospitalization rate at 6.0% (95% confidence interval [CI], 5.0% to 7.1%). Overall, the best PLT model reduced rates of hospitalization for severe COVID-19 by 1.6%, compared to the observed rate (3.7%) using standard clinical approaches during fall and winter 2021, the authors said.
The top-performing PLT led to the greatest-expected reduction in hospitalizations when giving mAbs to patients who were not fully vaccinated, had cardiovascular disease, healthy immune systems, and obesity.
In a commentary on the study, Johnathon Leider, PhD, and colleagues from the University of Minnesota and the Minnesota Department of Health explore the ethical considerations to machine-based learning and treatment allocations.
In a world with massive data, we have an obligation to follow paths toward the best outcome, all while making sure we promote equity and foster trust.
"In a world with massive data, we have an obligation to follow paths toward the best outcome, all while making sure we promote equity and foster trust. That is no small task," said Leider. "Researchers must consider how novel policy approaches might be received or implemented before these approaches will be actionable or practical and go well beyond the statistics."