A phase 3 randomized, controlled trial in adults in eight countries concludes that a protein-based vaccine targeting both the wild-type and Beta SARS-CoV-2 spike proteins is an estimated 75.1% effective against symptomatic COVID-19 among previously infected people and 30.9% among those never-infected amid Omicron variant predominance.
The researchers said the findings, published yesterday in The Lancet Respiratory Medicine, suggest that vaccines developed with an antigen from a non-dominant SARS-CoV-2 strain can provide cross-protection against newer variants.
75% were previously infected
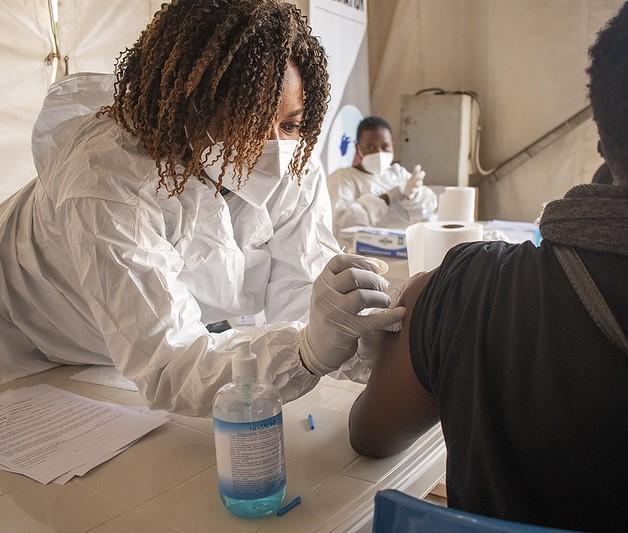
Scientists from vaccine manufacturer Sanofi led the study of the VidPrevtyn Beta vaccine involving 12,924 participants at 54 clinical research centers in Colombia, Ghana, India, Kenya, Mexico, Nepal, Uganda, and Ukraine from October 2021 to February 2022.
Participants were randomly assigned to receive two intramuscular 0.5-milliliter injections 21 days apart of either the bivalent (two-strain) vaccine with AS03 adjuvant (immune booster) from GSK (to increase the immune response; 6,472 participants) or a placebo (0.9% normal saline; 6,452).
A total of 58.4% of participants were men, 75.0% had a previous infection, and 89.3% received two injections. Follow-up was a median of 85 days after the first dose and 58 days after the second.
"COVID-19 vaccines with alternative strain compositions are needed to provide broad protection against newly emergent SARS-CoV-2 variants of concern," the study authors wrote.
'Could confer cross-protection'
At least 14 days after dose 2, 121 symptomatic COVID-19 infections were reported (32 vaccinees and 89 placebo recipients), for an overall vaccine effectiveness (VE) of 64.7% (95% confidence interval [CI], 46.6% to 77.2%). VE against symptomatic COVID-19 was 75.1% (95% CI, 56.3% to 86.6%) in previously infected participants and 30.9% (95% CI, –39.3% to 66.7%) in COVID-naive participants.
These findings suggest that vaccines developed with an antigen from a non-predominant strain could confer cross-protection against newly emergent SARS-CoV-2 variants, although further investigation is warranted.
Genome sequencing identified the infecting strain in 56.2% of 121 cases (Omicron BA.1 and BA.2, 63; Delta, 4; and both Omicron and Delta, 1).
Serious adverse events were rare. In a reactogenicity subset with data, solicited injection-site and systemic reactions within 7 days occurred in 1,398 (57.8%) of 2,420 vaccinees and 983 (40.9%) of 2,403 placebo recipients. One or more serious adverse events occurred in 30 (0.5%) vaccine recipients and 26 (0.4%) placebo recipients.
"These findings suggest that vaccines developed with an antigen from a non-predominant strain could confer cross-protection against newly emergent SARS-CoV-2 variants, although further investigation is warranted," the researchers wrote.
Lack of single-strain comparator
In a related commentary, Keith Chappell, PhD, of the University of Queensland in Australia, said that although the study authors show that the bivalent vaccine helps protect against symptomatic infection, "the absence of a monovalent comparator unfortunately means that attributing added protection to the inclusion of the beta variant is pure speculation at this point."
Chappell said the results confirm yet again the value of additional COVID-19 booster doses, even when they don't match currently circulating variants.
"The results of this phase 3 clinical trial are being published a full 2 years after the beta variant was fully replaced by the delta (B.1.617.2) variant, which was then subsequently replaced by omicron variants," he wrote. "The intervening period represents the time needed to switch to the manufacture of a new vaccine and fully validate its efficacy, and highlights the futility of attempting to release COVID-19 vaccines into widespread use that match circulating strains."
One option, Chappell said, is to regularly switch vaccines to match circulating SARS-CoV-2 strains, as is the case for seasonal flu vaccines, without waiting for formal effectiveness assessment.
With concerns around the severity of side-effects cited as a primary reason for vaccine booster hesitancy, improved tolerability is an important attribute.
But "updated vaccines are likely to be first distributed in high-income countries, further exacerbating the issue of inequality," he wrote. "Furthermore, routinely updating vaccines favours mRNA vaccines, for which the manufacturing process is easier to adapt and disadvantages protein-based subunit vaccines."
Chappell said that without clear data showing improved effectiveness of strain-matched vaccines, there is a risk that focusing on updates to vaccine antigen composition may overlook other alternatives with unique advantages.
The advantages of protein-based subunit vaccines include the lower rate of solicited systemic reactions. "With concerns around the severity of side-effects cited as a primary reason for vaccine booster hesitancy, improved tolerability is an important attribute," he concluded. "Liquid stability of 12 months at 2–4 °C is another important advantage of protein subunit vaccines, which could aid distribution to the 29.7% of the world's population yet to receive a COVID-19 vaccine."