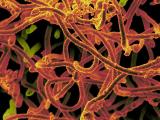
Federal officials are finalizing details on Ebola screening steps for travelers arriving at US airports, which may be announced in a few days and may resemble the kinds of questions that outbreak countries are asking departing passengers, Centers for Disease Control and Prevention (CDC) Director Tom Frieden, MD, MPH, said today.
The risk of another travel-linked Ebola case, such as the one in Texas, can never be reduced to zero until West Africa's outbreak is extinguished, he said at a media telebriefing today. But he said the CDC and other government agencies are taking a hard look at additional steps, focusing on ones that won't hamstring the response process underway overseas.
The three main outbreak countries have so far screened about 36,000 people departing on airlines, with three fourths of them bound for destinations outside the United States. The CDC has trained airport screeners in Guinea, Liberia, and Sierra Leone, which have flagged 77 people with fever and 3 people with other symptoms. As far as the CDC knows, none of the people with fever had Ebola, and most had malaria, a common illness in that part the world, Frieden said.
"I can assure you we will take additional steps, and the details will be worked out and announced in a few days," he added.
Senator suggests screening steps
US Sen. Charles Schumer, D-N.Y., issued a statement today saying he spoke with Frieden about tougher screening at US airports and is pleased that the CDC is preparing to implement some new steps. Schumer outlined a host of suggestions in an Oct 5 letter to the CDC and Customs and Border Protection (CBP).
He said the CDC could train CBP agents to actively screen passengers for fever if their travel originated from a West African outbreak country. Health officials have said fever screening can't identify all patients infected with Ebola. For example, the Liberian patient in Texas didn't start having symptoms until 4 days after he arrived in the United States.
Schumer also suggested that passengers arriving from the affected countries should fill out a detailed health form to pinpoint any Ebola exposure they had before arriving in the United States. He also urged the CDC and CBP to rigorously screen people working on cargo ships at entry ports, especially since Liberia has the world's second largest cargo ship fleet. Though experts have said a universal travel ban won't keep the disease out, he said, temperature checks and screening on US soil could be an acceptable middle ground.
Schumer has also urged the Department of Homeland Security to create a searchable database of passengers flying to and from West Africa, directly and indirectly, and share it with the nation's hospitals, which could help them avoid missing that risk factor, as occurred during the Texas patient's first visit to the emergency department.
Texas patient's condition still critical
At today's media briefing, David Lakey, MD, commissioner of the Texas Department of State Health Services (TDSHS), said none of the 48 patients who are being monitored for Ebola in Texas have fevers or other symptoms of the disease. The state is monitoring 10 people who had direct contact with the patient and 38 who were thought to have low-risk contact.
Texas Health Presbyterian Hospital said today that the man remains in critical condition and is on a ventilator and receiving kidney dialysis. Official said his liver condition declined over the weekend and subsequently improved, but his doctors have said that it could vary in coming days. The hospital added that the main continues to receive the investigational antiviral drug brincidofovir, which he began taking on Oct 4.
Spain details contact tracing, probes health worker case
Elsewhere, Spanish health officials have said a second test has confirmed an Ebola infection in a health worker who got sick after assisting with the care of a Spanish priest who was flown to a Madrid hospital after he was infected in Sierra Leone. The nurse's infection, announced yesterday by Spain's health ministry, is the first local transmission of the disease outside West Africa. The priest died on Sep 25, a few days after he arrived back in Spain.
The nurse, a woman, is a "sanitary worker" who entered the sick priest's room twice, according to media reports yesterday.
Three other people have been hospitalized in connection with the sick Spanish health worker, Reuters reported today. They include the woman's husband and two other people, one of whom is another health worker. A separate Reuters report said the other health worker, who had diarrhea but no fever, has tested negative for Ebola.
The European Centre for Disease Prevention and Control (ECDC) said in a statement on the case that most of the woman's contacts are medical staff, but some are family members. It said two ECDC experts are being deployed to Spain to help investigate how the woman was infected.
In a related development, the European Commission has asked Spain's health ministry to clarify how the health worker was infected, Agence France-Presse (AFP) reported today. Spain's health ministry is investigating the woman's infection, according to several media reports.
Spain's government has announced plans to euthanize the woman's dog, the Associated Press (AP) reported today. At today's CDC media briefing, Frieden, when questioned about that development, said he's aware of only one study in the medical literature about dogs and Ebola infection, which found dogs may have antibodies to the virus. He said in rural Africa, Ebola can infect mammals, and is probably spread by bats, which are mammals. Lakey said no potentially infected dogs have been identified in connection with the Texas case.
Other developments
- The World Health Organization (WHO) today said it is pulling together a 14-member expert group for informal consultation on the science to guide its Ebola outbreak response. It said the team will review the current science and information emerging from the outbreak countries. The WHO said it may use the expert observations to consider any changes in control steps immediately or after better data are available or to help gather data needed to guide decision making. The group's first meeting will take place by teleconference, with subsequent meetings depending on the WHO's needs. Peter Piot, MD, PhD, a London School of Hygiene and Tropical Medicine researcher who helped identify the Ebola virus in 1976, will lead the first meeting.
- An assessment of health infrastructure and emergency preparedness in four of Liberia's remote southeastern counties in mid August before any Ebola cases had been detected found only three physicians to cover all four counties, with physicians and some nursing staff having abandoned their posts and others still working, though they had not been paid in 3 months, according to an article in Morbidity and Mortality Weekly Report (MMWR). Hand washing stations were scarce, with some consisting of just a bamboo stem filled with water. Though the counties had Ebola task forces, limited resources and communications problems hampered community mobilization efforts. The team identified one suspected Ebola death and a confirmed death that involved the area's first instance of secondary transmission. The group said more Ebola cases have since been detected in the area and Ebola preparedness has improved, with task forces meeting and an incident command system in place. But they emphasized that the counties urgently need equipment and staff to do contact tracing, case management, and other tasks.
- In an effort to speed the development of safe and comfortable personal protective equipment (PPE) and other tools to help healthcare providers in West Africa battle Ebola, the US Agency for International Development (USAID) today launched a technology competition to fund and test innovations in infection control and a Web portal to help incubate new ideas about how to deliver care and stop the disease. USAID first announced the PPE challenge at a global health security summit in Washington, DC, on Sep 26.
- Though there are no regulations or recommendations about donations of blood and other human substances by people in the European Union who have recovered from Ebola infections, been exposed to the virus, or have traveled in outbreak regions, asymptomatic travelers should be barred from donating blood or other substances for 2 months after leaving outbreak areas, the ECDC said yesterday in a risk assessment. However, if organ transplantation is urgently needed, the period can be reduced to 1 month if the donor tests negative for Ebola. Contacts should be excluded from donating blood and other substances for 2 months beginning at the start of the monitoring period, and those who have recovered should not donate for 12 months, in line with guidance for viral hemorrhagic fevers. Also, the ECDC said living and deceased people who recovered from Ebola should have tested negative for Ebola in donation situations. The agency noted that its recommendations don't apply to blood collected from convalescent patients for use in treating Ebola infection.
See also:
Oct 7 Sen Schumer press release
Oct 7 Texas Health Resource statement
Oct 7 Reuters report on Ebola testing of second Spanish health worker
Oct 7 AFP story
Oct 7 ECDC statement
Oct 7 AP story
Oct 7 WHO statement
Oct 7 MMWR report
USAID Ebola Grand Challenge Web portal
Oct 6 ECDC technical report on Ebola transmission risk and donated blood and other substances