Nov 1, 2012
Serologic study suggests 20% of Americans were infected during 2009 pandemic
A serologic survey by the US Centers for Disease Control and Prevention (CDC) suggests that about 20% of the US population, including more than half of school children, were infected with the pandemic H1N1 (pH1N1) flu virus in 2009, says a report in PLoS One. The researchers used a baseline sample of 1,142 serum specimens from the 2007–08 National Health and Nutrition Examination Survey (NHANES). For a post-pandemic survey, they used 2,759 serum specimens submitted for routine screening to clinical diagnostic labs in New York City and nine states in December 2009 and January 2010. They defined seropositivity as an antibody titer of 40 or higher on hemagglutination inhibition assay. To adjust for the effects of pH1N1 vaccination, the team used CDC surveys of vaccination coverage in the affected states. The researchers found an overall rate of seropositivity to pH1N1 of 36.9%. After adjusting for the effects of pH1N1 vaccination, baseline cross-reactivity to the virus, and other factors, the researchers estimated the overall incidence of pH1N1 infection by the end of 2009 at 20.2%. Estimates varied greatly by age, with an incidence of 53.3% in children aged 5 to 17 years and a much lower level in elderly people. Applied nationwide, the findings suggests that 61.9 million people may have been infected.
Oct 31 PLoS One report
Intense exposure likely key factor in 2009-10 New York mumps outbreak
Long hours of intense face-to-face study in Orthodox Jewish boys at yeshiva schools likely played an important role in mumps outbreaks that affected certain New York communities in 2009 and 2010, according to a report today in the New England Journal of Medicine. Though young people in the affected communities had high vaccination rates, researchers suspect that the intensive exposure overcame vaccine-induced protection in the patients. Health officials recorded 3,502 outbreak cases from late June of 2009 through late June of 2010. Orthodox Jews made up 97% of the case-patients, with adolescents and males disproportionately affected. Among the adolescent patients, 89% had previously received two doses of vaccine against mumps. Researchers noted that the school days can last as long as 15 hours in yeshivas, where students practice an interactive form of study that requires students to sit across from each other at narrow tables for long hours, which they said could have allowed the efficient transmission of mumps virus. Health officials didn't see much sustained transmission outside the Orthodox community, though they noted that transmission patterns shifted over time from adolescent boys toward older and younger contacts of both sexes, suggesting that the infected boys introduced the virus into their homes. Investigators said the outbreak highlights the importance of high rates of two-dose vaccine coverage in all communities.
Nov 1 N Engl J Med abstract
Texas West Nile cases in last decade followed 3-year pattern
Texas recorded 2,274 West Nile cases from 2002 through 2011, two thirds of which involved neuroinvasive disease and 6% of which were fatal, according to a report in Emerging Infectious Diseases yesterday. The report also found that peaks occurred every 3 years. In an analysis of all cases reported to the state's health department, researchers estimated that the disease in that span cost the state $112 million, and the risk of contracting West Nile was highest in northwestern Texas, where Culex tarsalis mosquitoes predominate. The team also found that the highest case count (735) was reported in 2003, with additional peaks in 2006 (354) and 2009 (115). That every-3-year pattern continued in 2012, with a new high already recorded for the state: 1,665 West Nile cases through Oct 30, according to statistics from the US Centers for Disease Control and Prevention (CDC).
Oct 31 Emerg Infect Dis report
Latest CDC West Nile cases
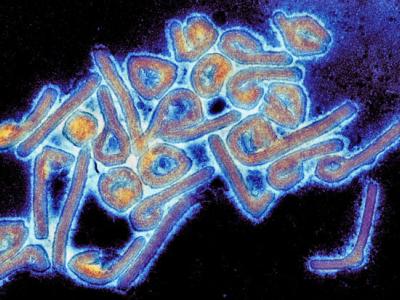
Hendra virus vaccine for horses debuts in Australia
The first vaccine for horses against potentially deadly Hendra virus infections recently launched in Australia, according to a report today from the International Business Times (IBT). The disease, first isolated in 1994 when it emerged in horses in Brisbane, is spread by bats to horses. Though rare, fatal infections have been reported in four humans, all of whom had exposure to sick or dead horses. The Hendra virus vaccine was developed by Pfizer and the animal health laboratory at Australia's Commonwealth Scientific and Industrial Research Organization, according to the report. It is being made available to veterinarians in Queensland and northern New South Wales, areas that have reported Hendra outbreaks. The vaccine is expected to cost from $130 to $220 per dose, and horses require a single shot followed by a booster 3 weeks later, IBT reported.
Nov 1 IBT story
Study: Early treatment important to tularemia success
In a case series of 139 tularemia patients from an epidemic in Turkey from December 2009 through August 2011, researchers found clinical success to be associated with early treatment, according to a report in Infection. Patients ranged in age from 6 to 83 years (mean, 43), and 60% were female. Disease manifestations were oropharyngeal (74%), glandular (16%), and oculoglandular (5%). Antibiotics (aminoglycosides, quinolones, and doxycycline) were used in 138 patients, and treatment failure was noted in 43 (31%). The investigators found significantly higher success rates with early treatment (P = 0.004) but found no difference between aminoglycoside and quinolone therapy. From those findings, the authors conclude, "Ciprofloxacin [a quinolone] is an effective and convenient choice in epidemics of tularemia, and early treatment is still the cornerstone of successful therapies."
Oct 28 Infection abstract