New research has found a small but steady increase in antibiotic use in sick children under the age of 5 in low- and middle-income countries (LMICs), with the biggest uptick seen in the world's poorest countries.
In a study published in The Lancet Global Health, a team of Swedish researchers analyzed data from 73 LMICs and found that reported antibiotic use among sick children under the age of 5 increased by 17% from 2005 through 2017. On average, around 4 in 10 sick children younger than 5 in these countries were reported to receive antibiotics for their illness in 2017.
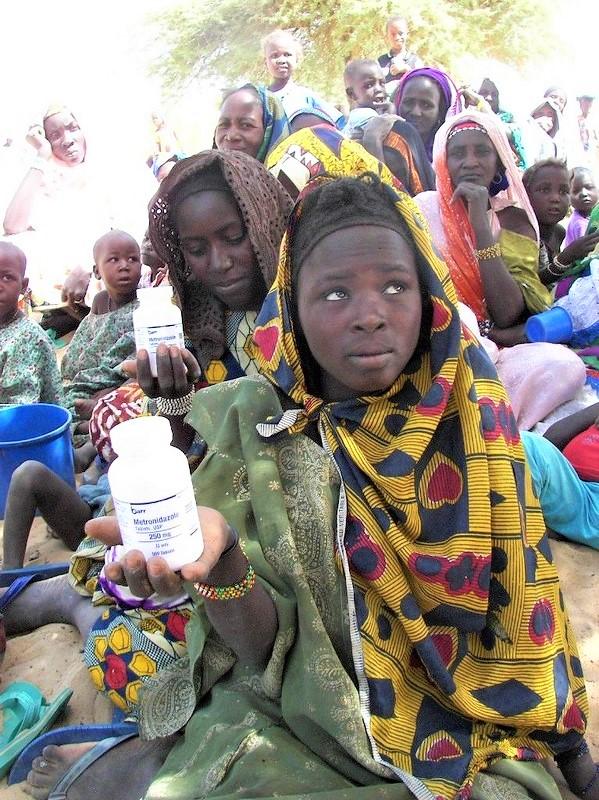
Among the countries analyzed, low-income nations, particularly those in Africa and Southeast Asia, saw the biggest jump in antibiotic use in sick kids (34%) during the study period, although these same countries had the lowest overall antibiotic use in preschoolers compared with other LMICs.
Almost 30% rate of recent illness
For the study, researchers from Uppsala University and the University of Gothenburg analyzed 132 Demographic and Health Surveys and Multiple Indicator Cluster Surveys carried out in 73 LMICs from 2005 through 2017. In these surveys, which are carried out every 3 to 5 years, women in each surveyed household are asked a series of questions about their children under 5, including questions about illnesses experienced by the children in the previous 2 weeks, and any medications used to treat the children.
While most assessments of global antibiotic consumption typically rely on pharmaceutical sales data, those data are often incomplete or unreliable in many LMICs. In addition, sales data don't always correspond directly to the number of antibiotic courses consumed by individuals. For these reasons, the researchers chose household surveys to fill in gaps on what is known about childhood antibiotic use in these countries.
Of the 132 surveys, 68 (51.5%) were from African countries, and 100 (75.8%) were from low-income and lower-middle-income countries. Altogether, the final data set included more than 1.5 million children under the age of 5, with 443,272 (29.4%) reported to have had either fever, diarrhea, or cough with fast or difficult breathing symptoms in the 2 weeks before the survey interview.
Analysis of the surveys found that reported antibiotic use among sick children under the age of 5 in the 73 LMICs increased from 36.8% (uncertainty interval [UI], 28.8% to 47.7%) in 2005 to 43.1% (UI, 33.2% to 50.5%) in 2017. The authors of the study note, however, that the results should be interpreted with caution because of the wide and overlapping UIs.
Low-income and lower-middle-income countries had the lowest reported antibiotic use in kids under 5 in 2017, with 39.5% in low-income countries (UI, 32.9% to 47.6%) and 41.7% (UI, 33.7% to 48.7%) in lower-middle-income countries, while upper-middle-income countries had the highest reported use: 59.2% (UI, 35.3% to 76.3%). Reported antibiotic use in LMICs in Europe (67.7%) and the Western Pacific region (61.7%) was nearly double that of countries in Africa (35.4%) and Southeast Asia (30.1%)
But the increase in antibiotic use in sick preschoolers over the study period was more pronounced in low-income countries, rising from 29.6% (UI, 21.2% to 41.1%) in 2005 to 39.5% (UI, 32.9% to 47.6%) in 2017. The increase in lower-middle income countries (from 40.7% to 41.7%) and upper-middle-income countries (55.9% to 59.2%) was much smaller.
The analysis also found that, among different symptom combinations reported in the surveys, antibiotic use was lowest when diarrhea alone was reported. Across LMICS, 33.4% (UI, 9.3% to 69%) of sick children with diarrhea alone reported antibiotic use in 2017, compared with 43.7% (UI, 12.2% to 82.6%) if fever alone was reported and 49.6% (UI, 14.3% to 84.5%) if cough with fast or difficult breathing alone was reported.
For each of those symptoms, reported antibiotic use in children was highest in the upper-middle-income countries. But over the study period, low-income countries saw the biggest increases in reported antibiotic use for fever symptoms alone (34%) and for cough with fast or difficult breathing symptoms alone (37%).
Access, appropriateness are issues
The authors of the study say the results are in line with previous assessments of global antibiotic consumption that have shown rising antibiotic use among all ages being driven by LMICs, a finding that's been attributed in part to rising per capita gross domestic product (GDP) rates in these countries and greater access to antibiotics.
But they also note that their estimates of antibiotic use in children in LMICs are significantly lower than shown a previous study, published in December 2019, which found that an average of 62.7% of sick children under 5 in LMICs received antibiotics from 2007 through 2016. The estimates of antibiotic use in that study, which focused on eight LMICs, were based on surveys from healthcare facilities.
"Although this difference in results could simply be due to differences between the studies as outlined, it could also reflect that the proportion of antibiotic use in the community is on the average, lower than that seen at health facilities," the authors write. "This is not unexpected, as many episodes of illness in the community go untreated, and only a fraction (often perceived as more serious) end up presenting to a health facility and hence are more likely to receive antibiotics."
In addition, they say the finding that antibiotic use in sick children under 5 was lowest in the low-income countries suggests that in these countries, lack of access to antibiotics may be still be a more significant issue than excessive use.
In an accompanying commentary, pediatric infectious diseases experts from St. George's University of London and the Swiss Tropical and Public Health Institute point out that how much of the antibiotic use reported in the study was appropriate is another issue that needs to be examined. Citing a recent study conducted in Tanzania that found that a large share of antibiotic prescriptions for children who had fevers were unnecessary, they argue that 40% antibiotic use in sick children under 5 is still probably more than what is needed for treatment of fever, diarrhea, and respiratory illnesses.
"Although quality of antibiotic use is difficult to assess, monitoring is essential to complement more quantitative measurements," they write. "Increasing access to antibiotics, as reported by Johansson and colleagues [authors of the new study] and others, could result in excessive and ultimately inequitable use, which excludes children most at need of antibiotic treatment."