Sep 28, 2005 (CIDRAP News) Hospital residents did poorly on a test of their ability to recognize and manage diseases potentially related to bioterrorism, but they fared much better after taking an online training program, according to a report in Archives of Internal Medicine.
The 631 physicians who participated in the study correctly diagnosed anthrax, smallpox, pneumonic plague, and botulism less than half the time, and they made correct management decisions only a quarter of the time, according to the report by Sara E. Cosgrove and colleagues from the Johns Hopkins University School of Medicine in Baltimore.
But the average scores on both tests rose to 79% after the residents completed the Web-based training program.
The 631 physicians were among 2,407 physicians in 30 internal medicine residency programs in 16 states and Washington, DC, who were invited to participate in the study. Thirty participants (4.8%) were attending physicians, and nearly all the rest were residents.
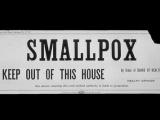
The physicians took a multiple-choice test on diagnosis and management of the four diseases before going through the training module. Afterward they took another test, with different questions. Anthrax, smallpox, botulism, and pneumonic plague are four of the six diseases or disease classes that terrorists are considered most likely to try to use.
On the diagnosis questions, the average pretraining score was 46.8%. The participants scored 70.5% on anthrax-related questions, 50.7% for smallpox, 49.6% for botulism, and 16.3% for pneumonic plague. After the training, the average diagnostic score improved to 79.0%.
On the management test, physicians scored an average of only 25.4% before training. They were right 60.2% of the time on botulism questions, but they scored only 14.6% on smallpox, 17.0% on anthrax, and 9.7% on plague. After taking the training, the overall average score soared to 79.1%.
In one common diagnostic error, after reading a description of a rash that was consistent with varicella, 42.6% of participants concluded it was smallpox. On the management side, more than 90% of participants knew the importance of quickly giving botulinum antitoxin for botulism, but 31.4% wrongly opted for giving antibiotics too.
The level of training didn't seem to affect the residents' scores, as first-, second-, and third-year residents all averaged about the same on the pretraining test, the report says. However, the attending physicians scored significantly higher than the residents, with an average score of 50.0% versus 36.9%. Geographic region had no apparent effect on the scores.
"The ability of physicians to distinguish smallpox, anthrax, botulism, and plague from other, more common disorders was poor, as was their ability to manage illness due to bioterrorism agents once a diagnosis had been made," the report states. One bright spot, however, was that most physicians could distinguish inhalational anthrax from other community-acquired pneumonias, probably because of publicity generated by the anthrax attacks of 2001.
One limitation of the study was that participants knew they were completing a training module on bioterrorism, which could have affected their diagnostic judgments, the report says. However, they were told that illnesses described might or might not be due to bioterrorism agents.
The authors say their findings suggest that the government should include physician education among its bioterrrorism preparedness priorities.
Cosgrove SE, Perl TM, Xiaoyan S, et al. Ability of physicians to diagnose and manage illness due to category A bioterrorism agents. Arch Int Med 2005;165(17):2002-6 [Full text]