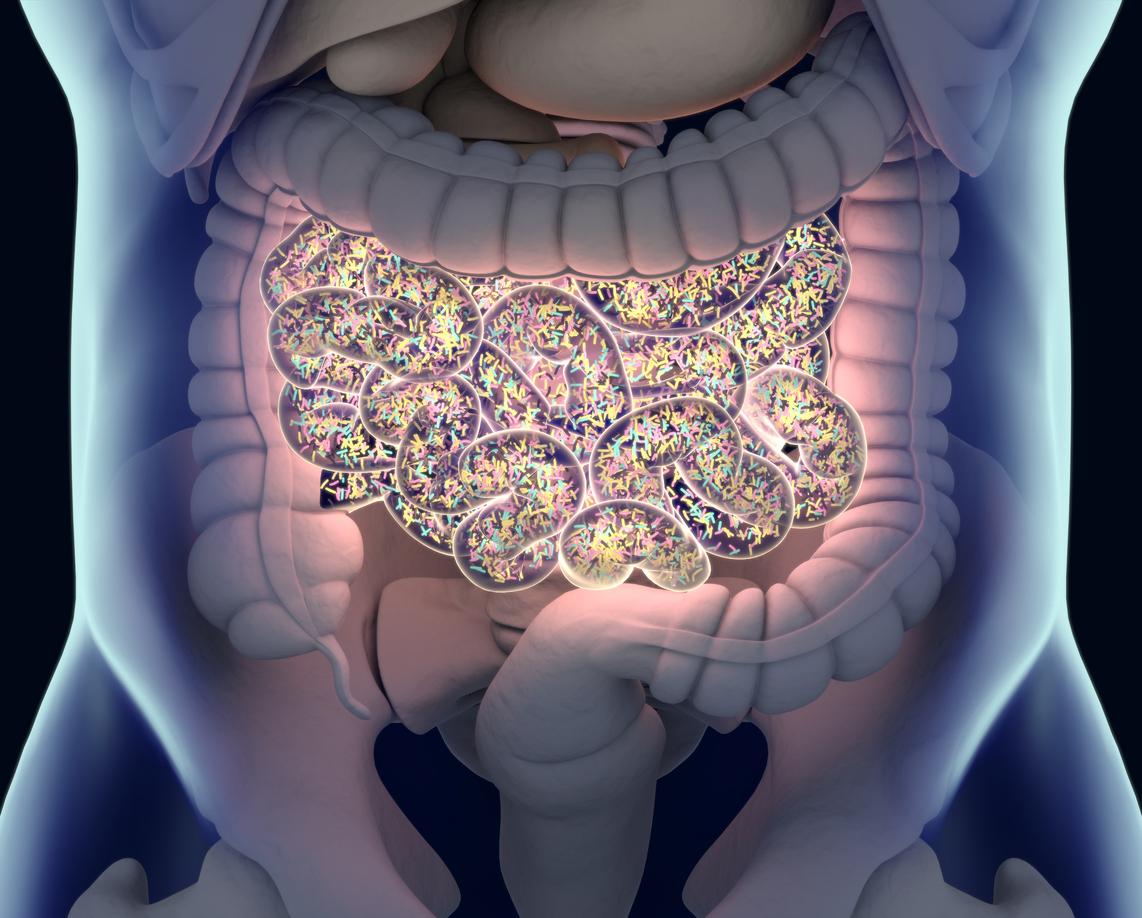
A study in Australia suggests the gut microbiomes of nursing home residents harbor hundreds of antibiotic resistance genes (ARGs), researchers reported yesterday in the Journal of Infection.
Conducted from March 2019 through March 2020 at five long-term aged-care facilities in South Australia, the study analyzed resident stool samples and medical records to define the gut resistome in nursing home residents and determine the relationship between antibiotic exposure and enteric ARG carriage.
Because of the challenges of diagnosing infections in the elderly and the higher likelihood of poor outcomes, widespread empiric antibiotic use is common in nursing homes, and residents experience disproportionate rates of drug-resistant infections. But little is known about asymptomatic carriage of resistance elements.
Doxycycline associated with high ARG abundance
Of the 164 residents (median age, 88; 71.9% women) who provided stool samples, 61% were prescribed antibiotics at least once in the prior 12 months (median prescriptions, 4), primarily for soft tissue, respiratory, or suspected urinary tract infections. The most commonly prescribed antibiotics were penicillins (33.5%), cephalosporins (32.3%), trimethoprim (22%), and doxycycline (12.8%).
Metagenomic analysis identified more than 1,100 unique ARGs conferring resistance to 38 antibiotic classes, including 20 ARGs of high clinical concern. Carriage of one or more ARGs of clinical concern was identified in 99% of participants.
Multivariate analysis found doxycycline exposure to be the greatest risk factor for high ARG abundance (adjusted odds ratio [aOR], 14.8; 95% confidence interval [CI], 5.3 to 40.9). High enteric ARG abundance was also associated with the number of separate antibiotic exposures (aOR, 6.4; 95% CI, 2.5 to 16.5), exposures within the prior 30 days (aOR, 4.6; 95% CI, 1.9 to 11.2) and prior 30 to 100 days (aOR, 2.6; 95% CI, 1.1 to 6.1), high duration of antibiotic exposure (aOR, 7.9; 95% CI, 3.1 to 19.9), and exposure to three or more antibiotic classes (aOR, 7.4; 95% CI, 2.9 to 18.6).
"Overall, the implications of our findings extend beyond individual treatment options," the study authors wrote. "They emphasise the importance of a holistic approach to antibiotic stewardship in long-term aged care settings, particularly in light of the expected surge in long-term aged care residency in the future."














