An analysis of antifungal use in US hospitals suggests a specific focus on antifungal stewardship may be warranted, researchers reported this week in the Journal of Antimicrobial Chemotherapy.
For the study, researchers from the Centers for Disease Control and Prevention (CDC) Mycotic Diseases Branch and the University of Texas MD Anderson Cancer Center used the Vizient Clinical Data Base to assess antifungal days of therapy (DOT) per 1,000 patient-days overall and by year at 412 US hospitals from 2018 through 2023. Because cancer is a common underlying condition in patients with invasive fungal infections (IFIs), they also compared antifungal use at hospitals with a National Comprehensive Cancer Network (NCCN) cancer center status and those without an NCCN-designated cancer center.
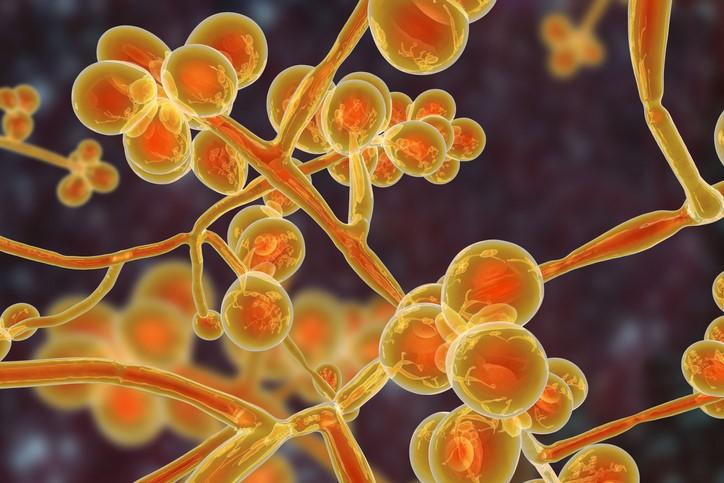
"Fungal infections cause substantial morbidity and mortality," the study authors wrote. "Monitoring antifungal use is a foundational aspect of antifungal stewardship, particularly as new disease-causing fungi emerge and antifungal resistance spreads."
4.5% of patients received antifungals
Of the nearly 40 million discharges analyzed, the proportion of patients who received any systemic antifungal was 4.5%, with azoles (3.8%) and echinocandins (0.9%) the most commonly prescribed antifungals. The overall antifungal DOT per 1,000 patient-days was 53.7 (114.5 among 25 NCCN hospitals and 43.2 among 387 non-NCCN hospitals), rising from 54.1 in 2018 to 55.0 in 2023.
Among patients who received an antifungal, the median age was 57.4 years, 30% had an IFI diagnosis code, and malignancy (35.4%) was the most common underlying condition. From 2020 through 2023, 5.7% of patients who received antifungals had a COVID-19 diagnosis.
The authors note that the proportion of patients who received an antifungal and the total antifungal DOT were nearly twice as high as reported in a 2006-2012 study that used a different data source, which could reflect rising numbers of patients susceptible to IFIs or methodological differences.
"Antimicrobial stewardship programmes have historically neglected antifungal medications, but the frequency of antifungal exposure coupled with the potential for resistance and high costs suggests that hospitals and patients may benefit from a specific focus on antifungal stewardship," they wrote.
















