- Amid indications that US Health and Human Services (HHS) Secretary Robert F. Kennedy Jr. is considering changes to the Vaccine Injury Compensation Program (VICP), the Infectious Diseases Society of America (IDSA) yesterday issued a statement reminding the public and policymakers that vaccines are responsible for some of the greatest gains in protecting people and increasing life expectancy and that access to vaccine should be strongly protected. The group added that serious vaccine-related injuries are rare, but when they occur, patients and families deserve the utmost care and compassion. The IDSA said it's important that VICP work as Congress intended, adding that any changes to improve the program should be made transparently with participation from Congress, specialty groups with expertise in vaccines, and patients. "Specifically, it is important that the VICP be funded appropriately to compensate injured individuals without putting an infeasible burden on vaccine manufacturers that could jeopardize severely the availability of safe and effective vaccines for the public," IDSA President Tina Tan, MD, said in the statement. Established in 1986 following concerns about a since-discontinued whole-cell pertussis vaccine, the VICP is designed to protect vaccine makers from most lawsuits alleging vaccine-related injury, while giving people claiming such injuries an opportunity to get a fair hearing and potentially receive compensation.
- Two Escherichia coli O157:H7 infections, one of them fatal, have been linked to venison—a rare source of the infection—from the same processing facility in Puryear, Tennessee, Food Safety News noted yesterday, citing a report from the Tennessee Department of Health. One of the patients is a 4-year-old girl from Tennessee who died from her infection in May. The investigation found a second case in a Texas resident who was sick in November and had a matching outbreak strain, and the only common food was venison from the processing facility. The Texas patient's family had traveled to Kentucky before she became ill. Investigators didn't find any violations at the producer, suggesting that the meat itself may have been contaminated.
- Federal health officials are investigating the sources of two Cyclospora outbreaks, one that has sickened 30 people and another that has sickened 41, the Food and Drug Administration (FDA) said in its latest Coordinated Outbreak Response and Evaluation (CORE) Network update. The illnesses were originally thought to have been linked to one outbreak, but epidemiologic information from state partners and the US Centers for Disease Control and Prevention suggests two distinct outbreaks. The FDA has started a trace-back investigation for the event with 30 cases identified so far. Foodborne infections from the Cyclospora cayetanensis parasite typically rise in the summer. Past outbreaks were linked to fresh produce, such as cilantro, basil, snow peas, and raspberries, but sometimes a specific source isn't identified. Profuse diarrhea that can last several weeks is the main symptoms of the disease, which is endemic in some tropical countries.
Quick takes: Concerns about changes to vaccine injury program, venison-linked E coli, 2 Cyclospora outbreaks
Study highlights antifungal use in US hospitals
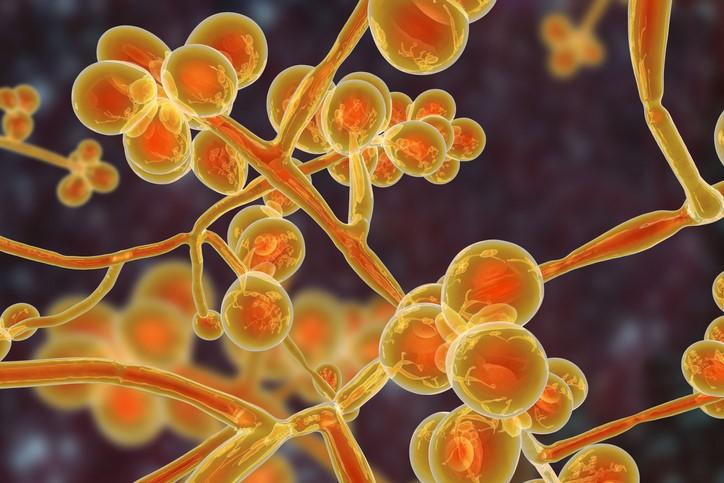
An analysis of antifungal use in US hospitals suggests a specific focus on antifungal stewardship may be warranted, researchers reported this week in the Journal of Antimicrobial Chemotherapy.
For the study, researchers from the Centers for Disease Control and Prevention (CDC) Mycotic Diseases Branch and the University of Texas MD Anderson Cancer Center used the Vizient Clinical Data Base to assess antifungal days of therapy (DOT) per 1,000 patient-days overall and by year at 412 US hospitals from 2018 through 2023. Because cancer is a common underlying condition in patients with invasive fungal infections (IFIs), they also compared antifungal use at hospitals with a National Comprehensive Cancer Network (NCCN) cancer center status and those without an NCCN-designated cancer center.
"Fungal infections cause substantial morbidity and mortality," the study authors wrote. "Monitoring antifungal use is a foundational aspect of antifungal stewardship, particularly as new disease-causing fungi emerge and antifungal resistance spreads."
4.5% of patients received antifungals
Of the nearly 40 million discharges analyzed, the proportion of patients who received any systemic antifungal was 4.5%, with azoles (3.8%) and echinocandins (0.9%) the most commonly prescribed antifungals. The overall antifungal DOT per 1,000 patient-days was 53.7 (114.5 among 25 NCCN hospitals and 43.2 among 387 non-NCCN hospitals), rising from 54.1 in 2018 to 55.0 in 2023.
Among patients who received an antifungal, the median age was 57.4 years, 30% had an IFI diagnosis code, and malignancy (35.4%) was the most common underlying condition. From 2020 through 2023, 5.7% of patients who received antifungals had a COVID-19 diagnosis.
The authors note that the proportion of patients who received an antifungal and the total antifungal DOT were nearly twice as high as reported in a 2006-2012 study that used a different data source, which could reflect rising numbers of patients susceptible to IFIs or methodological differences.
"Antimicrobial stewardship programmes have historically neglected antifungal medications, but the frequency of antifungal exposure coupled with the potential for resistance and high costs suggests that hospitals and patients may benefit from a specific focus on antifungal stewardship," they wrote.
Infections with high-risk HPV strains 16/18 less than 1% after vaccination rollout, data suggest

Human papillomavirus (HPV) vaccination has nearly eliminated infection with the high-risk HPV strains 16/18, which cause over 70% of cervical cancer, in Danish women immunized as adolescents, suggests a study published in Eurosurveillance.
Researchers assessed the HPV content of up to three cervical samples from 8,659 women aged 22 to 30 years screened from February 2017 to February 2024, 90% of whom had received three doses of the quadrivalent (four-strain) HPV vaccine starting in 2008, when the country began offering free vaccination to girls turning 12. Danish women are screened for cancer from ages 23 to 64.
In 2017, Denmark switched to a nine-valent HPV vaccine, which prevents up to 90% of cervical cancers. Since 2016, a two-dose regimen has been used in girls younger than 15 years, while three doses are still given to those aged 15 and older.
"Compared with previous generations, these women are expected to have a considerably lower risk of cervical cancer and it is pertinent to assess the new generations' future need for screening," the authors wrote.
The team then compared HPV prevalence, persistence, and incidence among vaccinated and unvaccinated women. Before the HPV vaccination program was launched, all cervical cancers showed evidence of high-risk HPV infection, with types 16/18 accounting for 74% of cases, they noted.
Less intensive but continued screening recommended
The prevalence of HPV types 16/18 in the samples fell from 15% to 17% before 2008 to less than 1% in vaccinated women in 2021, but the prevalence of these types in unvaccinated women stayed at 5%, down from 17% to 19% before vaccine availability, which the researchers say "strongly indicates population immunity."
Our study provided solid, real-world evidence of stable protection against HPV16/18.
Roughly one third of women screened were still infected with high-risk HPV types not covered by the vaccines, and these cases were more common in vaccinated than in unvaccinated women, although at a low level.
"Our study provided solid, real-world evidence of stable protection against HPV16/18," the authors concluded. "The high but steady proportion of women infected with high-risk HPV types not covered by the vaccine indicate a need for less intensive but continued screening of these generations."












