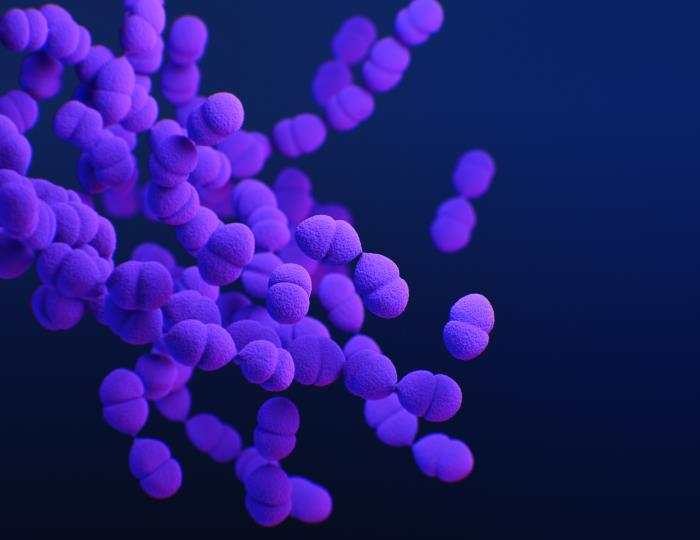
Higher levels of social vulnerability may increase the likelihood of having a resistant Streptococcus pneumoniae infection, researchers reported yesterday in Clinical Infectious Diseases.
Using S pneumoniae isolates collected from hospitalized and ambulatory patients at 177 US facilities from 2011 through 2022, researchers from Merck and Becton, Dickinson & Company evaluated associations between antibiotic resistance and the social vulnerability index (SVI). Created by the Centers for Disease Control and Prevention and the Agency for Toxic Substances and Disease Registry, the SVI measures four themes that contribute to social vulnerability: socioeconomic status (SES), household characteristics, racial and ethnic minority status, and housing type and transportation.
Of the 8,008 S pneumoniae isolates collected from 574 US counties in 39 states, the overall rate of antimicrobial resistance (AMR) was 49.9%, with 13.4% of isolates reported as multidrug-resistant. A multivariable analysis found that higher SVI scores were associated with increased risk of AMR, with the strongest links found for SES and household characteristics.
On average, a decile increase of SES, indicating greater vulnerability, was associated with a 1.28% increased risk of AMR (95% confidence interval [CI], 0.61% to 1.95%). A decile increase of household characteristic score, indicating household members ages 17 and younger or 65 and older, was associated with a 0.81% increased risk of AMR (95% CI, 0.13% to 1.49%).
No associations were found with racial and ethnic minority status, housing type and transportation, or overall SVI scores.
More pneumococcal vaccination could help
Resistant S pneumoniae infections account for roughly 830,000 deaths globally each year. The authors say that, in addition to shedding light on the role that social vulnerability may play in increasing the risk of acquiring a resistant S pneumoniae infection, the findings have important implications for pneumococcal vaccination, which has proven to be an effective strategy for reducing pneumococcal disease, including infections caused by resistant S pneumoniae strains.
"Important strategies to combat increasing SP [Streptococcus pneumoniae] AMR are increasing vaccination coverage, especially in those communities that face health inequities, as well development of vaccines with broader coverage of serotypes observed in adults," they wrote.















