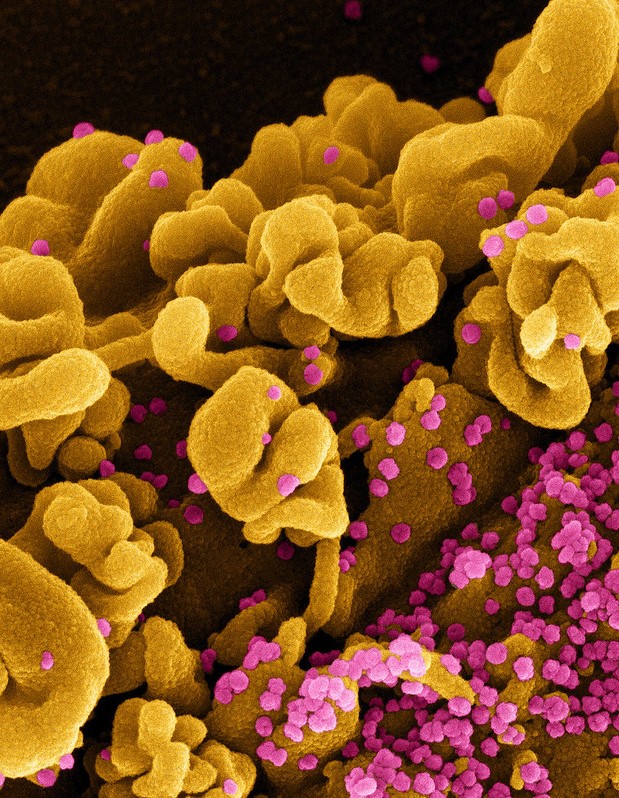
Menstrual cycles may lengthen by up to 1 day following COVID-19 vaccination, but the effect is temporary and vaccination makes little difference in cycle regularity, bleed length, heaviness of bleed, or menstrual pain, according to a study yesterday in Vaccine.
Menstrual cycles may lengthen by up to 1 day following COVID-19 vaccination, but the effect is temporary and vaccination makes little difference in cycle regularity, bleed length, heaviness of bleed, or menstrual pain, according to a study yesterday in Vaccine.
Since COVID-19 vaccines were first introduced for emergency use in North America in early 2021, women have shared anecdotal accounts on social media that their menstrual cycles changed following vaccination.
This prospective cohort study was based on the cycles of 1,137 participants who enrolled in Pregnancy Study Online (PRESTO), a preconception cohort study of couples trying to conceive, during January 2021 to August 2022. The women were not using fertility treatments, were ages 21 to 45, and lived in the United States or Canada.
The participants completed surveys at baseline and every 8 weeks for up to 12 months. They answered questions on vaccination and menstrual cycle characteristics, including cycle regularity, cycle length, bleed length, heaviness of bleed, and menstrual pain.
At the beginning of the study, no participants had been vaccinated against COVID-19. Participants either completed 6 follow-up questionnaires (13.8%), conceived before 12 months (64.6%), initiated fertility treatment (11.1%), stopped trying to conceive (2.0%), or were lost to follow-up or withdrew from the study (8.5%).
Short-term changes in menstrual cycle characteristics likely do not translate into meaningful differences in fertility.
A total of 437 participants (38.4%) received at least one COVID-19 vaccine dose during the study.
The only statistically significant finding was an average 1.1-day-longer menstrual cycles after receiving the first dose of COVID-19 vaccine (95% confidence interval [CI], 0.4 to 1.9) and an average 1.3-day-longer cycles after receiving the second dose (95% CI, 0.2 to 2.5). There were no changes to bleeding or pain, and by cycle two following vaccination the participants reported a return to their baseline.
"Taken together, these results indicate that short-term changes in menstrual cycle characteristics likely do not translate into meaningful differences in fertility," the authors concluded.
 A new
A new