A study today of patients with Klebsiella pneumoniae infections in one of the nation's largest cities has found that a relatively rare strain of the hospital superbug was responsible for more than one third of resistant K pneumoniae infections.
In mBio, researchers report that 35.7% of 1,777 drug-resistant K pneumoniae strains cultured from patients at Houston's Methodist Hospital System belonged to clonal group 307 (CG307), a clade—or subgroup—of strains that's been sporadically identified in other parts of the world but about which little is known. A little more than a fourth of the infections (26.7%) were caused by CG258, the clonal group responsible for most of the drug-resistant K pneumoniae infections in the United States.
"This was an extremely surprising finding," lead author James Musser, MD, PhD, chair of the department of pathology and genomic medicine at Houston Methodist, told CIDRAP News.
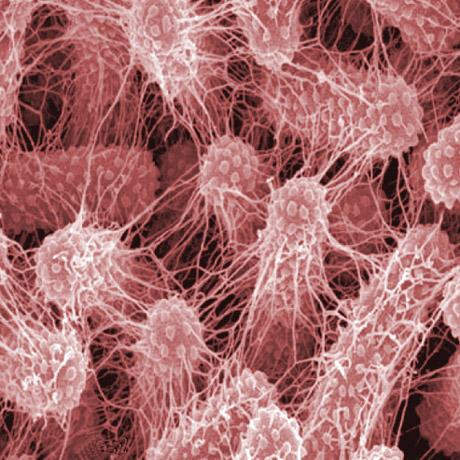
K pneumoniae is a gram-negative bacterium that is normally found in the human intestines but can cause a host of healthcare-associated infections—including pneumonia, bloodstream infections, and wound infections—in hospital patients and can be deadly when it is resistant to the drugs used to treat it. In recent decades, drug-resistant K pneumoniae has emerged as a major healthcare-associated infectious agent in US hospitals and around the world.
Levels not seen before
To get a better understanding of this pathogen and its "genetic face," Musser and researchers from the Argonne National Laboratory and the University of Chicago sequenced the genomes of 1,777 extended-spectrum beta-lactamase (ESBL)-producing strains cultured from infected patients at Houston Methodist hospitals from September 2011 through May 2015. ESBL-producing K pneumoniae are resistant to antibiotics such as penicillin and cephalosporins.
Decoding and analyzing the genome of these K pneumoniae strains revealed that they were broadly classified into three main genetic clades: CG307, CG 258, and a genetically heterogeneous array of strains known to have caused infections around the world. Clades are essentially clans, a group of related strains originating from a common ancestor.
While CG307 strains have been identified in parts of Europe, Asia, Africa, and South America, Musser said, they've never before been seen in such abundance in one city, anywhere.
"Certainly it's been described sporadically elsewhere," Musser said, "but not to the numerical dominance we see here in Houston." Part of that is the fact that no studies of this magnitude have been conducted in other urban areas.
Why is this uncommon clonal group so abundant Houston? That's the question that remains unanswered, although Musser suggested the diversity of the city's 6 million residents might play a role.
"It's important to understand now that Houston is the most ethnically diverse city in the US, officially," he said. "There's huge flux through our port, there's huge flux to Central and South America, there's huge flux to Southeast Asia…so the fact that we've got a different strain story, although surprising…is not a big shock."
Array of resistance genes, including NDM-1
Genome sequencing further showed that the CG307 strains, like CG258 strains, carry a diverse array of resistance genes, including genes harboring enzymes that confer resistance to carbapenem antibiotics, considered a last-resort therapy for drug-resistant infections. They also harbor multiple plasmids, the mobile pieces of DNA that can transmit resistance genes to other K pneumoniae bacteria and other types of bacteria, like Escherichia coli.
One of the genes identified in a CG307 strain was NDM-1, a carbapenem-resistance gene that is mainly found in India, can be easily transferred between strains by plasmids, and confers resistance to nearly all beta-lactam antibiotics. K pneumoniae strains carrying NDM-1 are very difficult to treat and can spread rapidly in hospitals.
"It's concerning to us to know that that strain is here somewhere in our community," Musser said.
In addition, experiments conducted on mouse models showed that CG307 strains appear to be just as virulent as CG258 strains, which is significant given that CG258 is the clonal group mainly associated with hospital outbreaks of carbapenem-resistant K pneumoniae.
"By every clinical value we measured, statistically, the CG307 are equivalent in virulence to the CG258," co-author S. Wesley Long, MD, PhD, associate director of Houston Methodist's clinical microbiology laboratory, said. The mouse experiments also suggested the body's immune response to the strains may be different, but more research is necessary.
Fortunately, all the CG307 strains identified remain susceptible to certain antibiotics, Long said, and they do not appear to be more drug-resistant or difficult to treat than CG258 strains. Among the patients with K pneumoniae infections, there was no statistically significant difference between the observed in-hospital mortality of patients infected with CG307 strains and those infected with CG258 strains.
Predicting drug resistance
Barry Kreiswirth, PhD, a founding director of Rutgers University's Public Health Research Institute Tuberculosis Center, calls the findings "very interesting."
"The clinical concern is whether this ESBL clone will be a problem if and when it becomes carbapenem resistant," said Kreiswirth, who's done extensive research on CG258. Another strain of carbapenem-resistant K pneumoniae that can quickly spread in healthcare settings would add to the superbug burden in US hospitals.
"This is a very thorough local epidemiological study of an important multidrug-resistant pathogen," Melissa Hargreaves, PhD, a research scientist at the Minnesota Department of Health, added. Hargreaves said that it would be interesting to apply the study methods to ESBL-producing K pneumoniae populations in other parts of the country.
Another notable outcome of the study is that, with the large set of whole-genome sequence data the researchers gathered, and some novel computational analysis, they were able to develop a classification system that predicted resistance for 12 of the 16 antibiotics tested. Musser said the hope is that, in the future, physicians will be able to pair this system with rapid sequencing technology to quickly determine drug resistance in K pneumoniae infections and initiate proper antibiotic therapy.
"Our goal is to be able to infer antimicrobial agent resistance as soon as possible and faster than can be done now with conventional antimicrobial susceptibility tests," Musser said. "We're working on that very extensively now."
See also:
May 16 mBio study