- The Florida Department of Health reported two more local malaria infections, raising its total to six, according to its latest surveillance report, which covers data for the week ending July 1. Both of the new cases were in Sarasota County, the same location as the previous four cases.
- Three African nations reported more polio cases this week, all involving vaccine-derived types, the Global Polio Eradication Initiative said in its weekly update. Burkina Faso reported its first circulating vaccine-derived poliovirus type 2 (cVDPV2) case of the year, which was in Gaoua. Chad reported 2 more cVDPV2 cases in different locations, putting its total for the year at 10. And Nigeria reported 6 more such cases from four different areas, raising its 2023 total to 16.
- Italy's health ministry yesterday reported that serology tests on dogs and one cat at a poultry farm in Brescia, located in northern Italy's Lombardy region, revealed that they likely experienced mild H5N1 avian flu, according to a statement translated and posted by Avian Flu Diary, an infectious disease news blog. The farm had experienced an H5N1 outbreak. Officials also said an analysis of the virus that infected the poultry found it was most similar to a virus found recently in gulls in northern Italy and that it had a mutation in the PB2 gene that suggests it may be more adapted to mammals.
Quick takes: More malaria in Florida, polio in Africa, avian flu in dogs and cat in Italy
Most US COVID-19 markers decline further
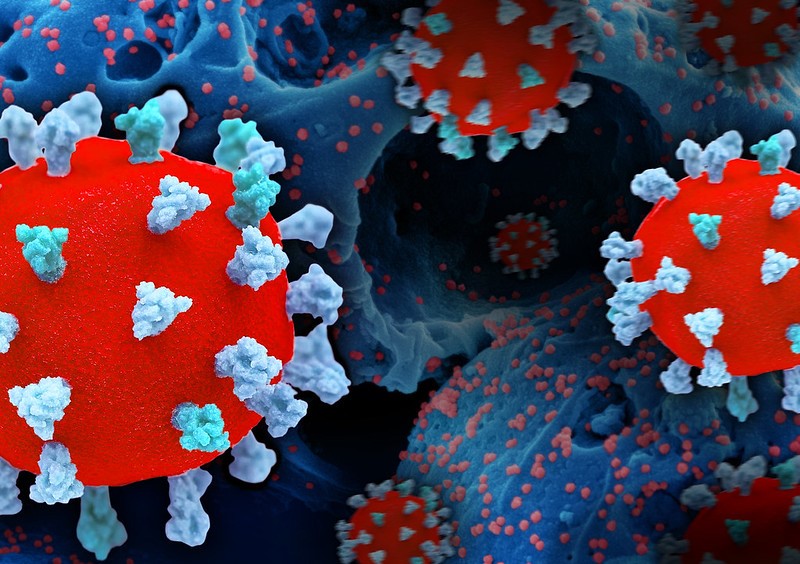 COVID-19 hospitalizations and deaths continue to decline, with levels down 5.9% and 9.1%, respectively, over the past week, the Centers for Disease Control and Prevention (CDC) said in its latest data update.
COVID-19 hospitalizations and deaths continue to decline, with levels down 5.9% and 9.1%, respectively, over the past week, the Centers for Disease Control and Prevention (CDC) said in its latest data update.
The measures that CDC uses as early markers, however, rose slightly. Emergency department visits for COVID were up 2% from a week ago, and test positivity rose by 0.4%. Hospitalization levels were high in only a few counties, two in southern Texas and two in central Montana. Test positivity was slightly higher in south-central, southwestern, and western states, as well as in New York.
Also, the CDC today updated its variant proportions, showing that levels of the Omicron XBB.1.5 subvariant continued to decline over the past 2 weeks, dropping from 26.3% to 16.1%. Meanwhile, proportions of a handful of other subvariants rose, including XBB.1.16, XBB.2.3, XBB.1.16.1, XBB.1.16.6, and EG.5.
FDA clears rapid diagnostic test for respiratory ailments
Australian diagnostics company Lumos Diagnostics announced this week that it has received US Food and Drug Administration (FDA) marketing clearance for a rapid diagnostic test that helps clinicians determine when antibiotics are needed for respiratory infections.
The FDA clearance means that FebriDX, a disposable point-of-care immunoassay designed to aid diagnosis of acute bacterial respiratory infections, can now be marketed in the United States for use by healthcare providers in urgent care and emergency care settings. Company officials say the test, which differentiates bacterial- from viral-associated host immune response and is intended to be used in conjunction with clinical signs and symptoms, could help improve antibiotic prescribing for acute respiratory infections.
We continue to believe it has an important role to play in antibiotic stewardship.
Although acute respiratory infections are predominantly viral in origin, they are the most common diagnosis for which outpatient antibiotics are prescribed.
"We are delighted to finally secure clearance to market our FebriDx rapid, point-of-care test in the US as we continue to believe it has an important role to play in antibiotic stewardship," said Lumos CEO Doug Ward in a company press release.
Increased antibiotic exposure linked to severe COVID-19 outcomes
 Repeated antibiotic exposure may be associated with severe COVID-19 outcomes, British researchers reported this week in eClinical Medicine.
Repeated antibiotic exposure may be associated with severe COVID-19 outcomes, British researchers reported this week in eClinical Medicine.
To investigate whether frequent antibiotic exposure may be linked to COVID-19 severity, a team led by researchers from the University of Manchester conducted a matched case-control study of patients hospitalized for COVID-19 (the cases) and those with a COVID-19 diagnosis (the controls). Using 3 years of patient data prior to infection, the researchers created five quintile groups based on the number of prior antibiotic prescriptions and used conditional logistic regression to compare the difference between cases and controls.
Overall, 2.47 million COVID-19 patients were identified from February 1, 2020, to December 31, 2021. Of those, 98,420 were hospitalized, and 22,600 hospitalized COVID-19 patients died within 30 days of admission.
The researchers observed a dose-response relationship between the number of antibiotic prescriptions and the risk of severe outcomes. The case group had higher odds of receiving antibiotics than controls, and the risk rose with increased exposure. For the highest antibiotic exposure quintile, the adjusted odds ratio (OR) was 1.80 (95% confidence interval [CI], 1.75 to 1.84) for hospital admission and 1.34 (95% CI, 1.28 to 1.41) for death compared with patients without antibiotic exposure.
Larger number of prior antibiotic types was also associated with more severe COVID-19 outcome. The adjusted OR for those who received more than three antibiotic types in the previous 3 years was nearly double that of those who received only one antibiotic type (OR, 1.80; 95% CI, 1.75 to 1.84 vs OR, 1.03; 95% CI, 1.01 to 1.05).
It seems advisable to discourage the regular practice of indiscriminately prescribing antibiotics repeatedly and intermittently.
The authors say that while the results could be subject to potential confounding—eg, patients using antibiotics may have been immunocompromised and more likely to be hospitalized for COVID-19—a possible explanation is that repeated antibiotic exposure may have disrupted the gut microbiota in ways that led to adverse events or increased risk of secondary bacterial infection.
"Given the known effects of antibiotics on the gut microbiome, it seems advisable to discourage the regular practice of indiscriminately prescribing antibiotics repeatedly and intermittently, given their uncertain benefits and likely risks," they wrote.
Study shows early COVID spike in antibiotic use in 3 South American countries
 Data from hospitals in Chile, Brazil, and Argentina show substantial increases in intravenous antibiotic use at the beginning of the COVID-19 pandemic, researchers reported this week in Clinical Infectious Diseases.
Data from hospitals in Chile, Brazil, and Argentina show substantial increases in intravenous antibiotic use at the beginning of the COVID-19 pandemic, researchers reported this week in Clinical Infectious Diseases.
For the ecological study, a team led by researchers from the US Centers for Disease Control and Prevention (CDC) calculated antibiotic use (AU) rates for intravenous antibiotics in acute care wards at six healthcare facilities (HCFs) in the three countries (two in each country) during two periods: March 2018 to February 2020 (prepandemic) and March 2020 to February 2021 (pandemic). They then compared the median AU during the two period and conducted an interrupted time series analysis to analyze changes in AU during the pandemic. All six HCFs reported having antibiotic stewardship programs.
Compared with the prepandemic period, the median AU rates significantly increased in four of the six HCFs during the pandemic period (percentage change, 6.7% to 35.1%). In the interrupted time series models, five of six HCFs saw significant increases in the use of all antibiotics combined immediately after the onset of the pandemic (immediate effect estimate range, 15.4 to 268), but only one of the five experienced a sustained significant increase in AU rate over time during the pandemic period. The effect of the pandemic onset varied by antibiotic and HCF.
The study authors say the high AU rates observed early in the pandemic are not surprising, given the uncertainty in the appropriate management of COVID-19 patients and concerns about secondary bacterial infections.
Although most increases were observed immediately after the onset of the pandemic, continued monitoring of [antibiotic use] in inpatient settings and understanding trends in antibiotic resistance in South America is important.
"Although most increases were observed immediately after the onset of the pandemic, continued monitoring of AU in inpatient settings and understanding trends in antibiotic resistance in South America is important to inform preventive actions," they wrote. "The COVID-19 pandemic demonstrated the need for HCFs to have pandemic preparedness plans that include implementing or strengthening both diagnostics and ASPs to mitigate overuse of antibiotics."













