A randomized controlled trial in Uganda found that seasonal malaria chemoprevention (SMC) with two different regimens effectively reduced malaria incidence in children under 5, with no safety concerns, researchers reported this week in The Lancet Infectious Diseases.
The three-arm, open-label, cluster-randomized trial, conducted in 2022 in a region of Uganda where malaria transmission is highly seasonal, enrolled and randomly assigned children in 380 villages 1:1 to receive SMC with sulfadoxine-pyrimethamine combined with amodiaquine (SPAQ) or dihydroartemisinin-piperaquine, and an additional 47 villages to a control group that received no SMC.
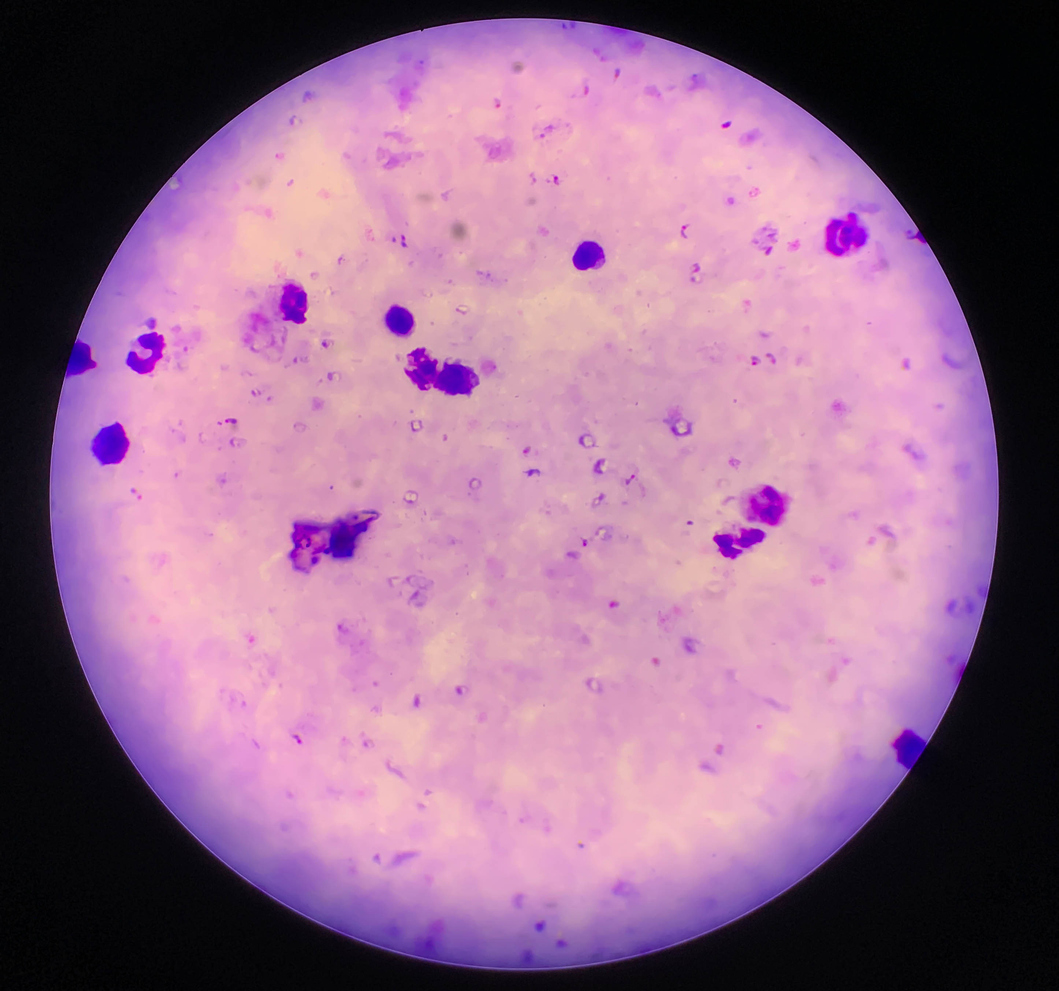
The primary end point was confirmed malaria incidence. While a previous trial found that SMC with SPAQ reduced malaria in children by 92%, concerns about parasite resistance to sulfadoxine-pyrimethamine in East and Southern Africa has prompted the need to evaluate alternative regimens.
Among the 3,881 children enrolled (1,755 in the SPAQ group, 1,736 in the dihydroartemisinin-piperaquine group, and 380 in the control group), malaria incidence rates were 0.90, 0.80, and 18.26 cases per 100 person-months, respectively. SPAQ and dihydroartemisinin–piperaquine reduced malaria risk by 94% (hazard ratio [HR], 0.06; 95% confidence interval [CI], 0.04 to 0.08) and 96% (HR, 0.04; 95% CI, 0.03 to 0.06), respectively, compared with the control group. Based on the prespecified non-inferiority margin of 1.4, there was non-inferiority between the protective effectiveness of dihydroartemisinin–piperaquine and that of SPAQ (HR, 0.90; 95% CI, 0.58 to 1.39).
Concerns about resistance remain
Although five mutations that mediate moderate sulfadoxine-pyrimethamine resistance were prevalent, mutations conferring high-level resistance were rare. No serious or fatal events were reported in the SPAQ group or the dihydroartemisinin–piperaquine group.
Trial investigators say that while the results are encouraging, parasite resistance remains a critical concern.
"Continued monitoring of drug resistance and exploration of alternative regimens are necessary to ensure the long-term effectiveness of SMC in areas with resistance to sulfadoxine–pyrimethamine," they wrote.










