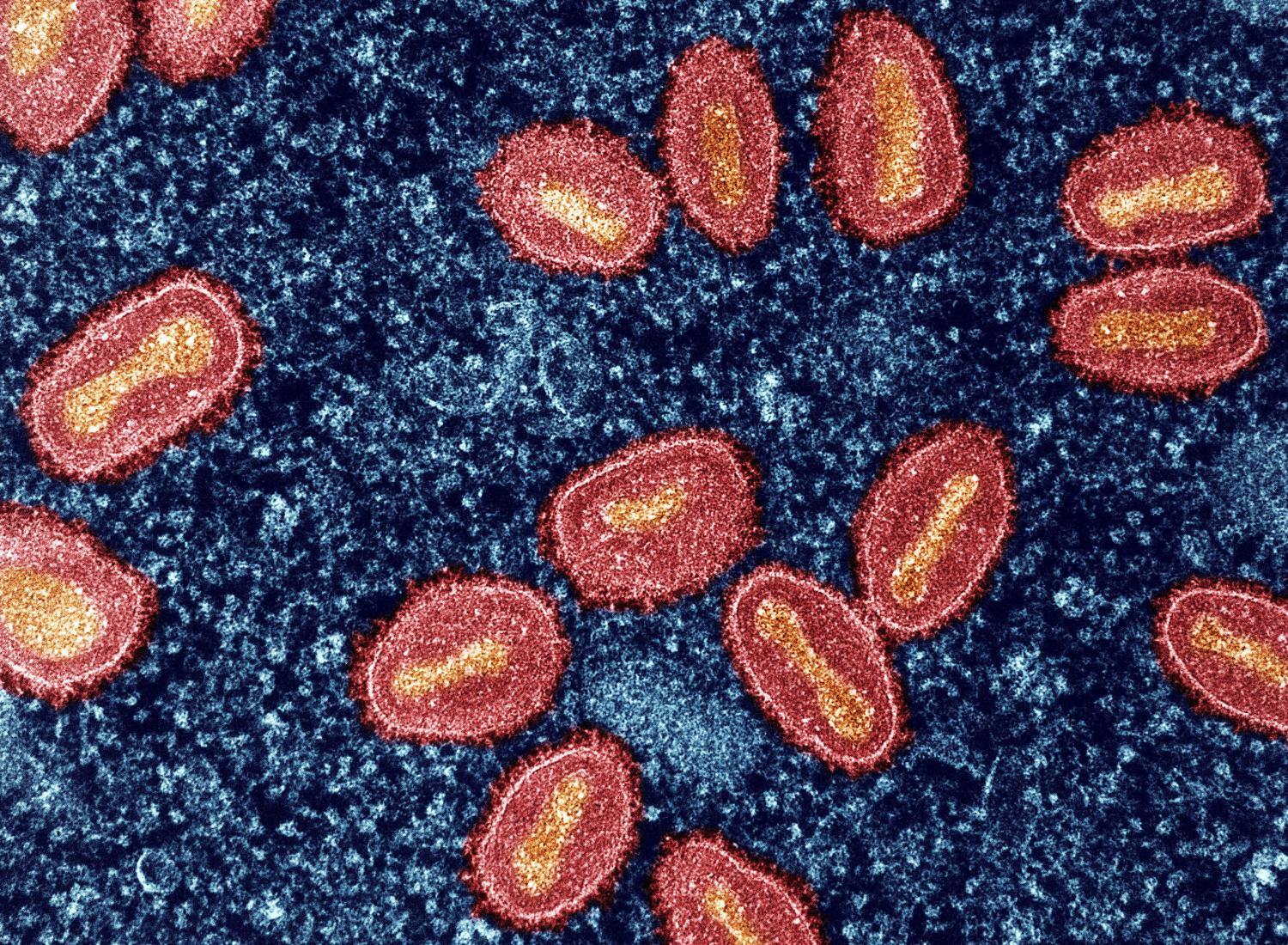
Though the 2022 mpox outbreak was primarily transmitted through sexual contact among men who have sex with men in the United States, close, nonsexual case contacts have contracted the virus, but data released today show that the risk is quite low.
Another mpox study today showed that dose-sparing vaccine administration of the Jynneos vaccine appeared to have worked.
Secondary nonsexual attack rate of 1.5%
In Morbidity and Mortality Weekly Report, data from nonsexual mpox case contacts in Tennessee and Washington, DC, show secondary attack rates of around 1.5%, suggesting follow-up is warranted in the 21 days following mpox exposure.
The study looked at US mpox case contacts reported from May 1 to July 31, 2022. Most jurisdictions in the United States did not report nonsexual case contacts during the period. Tennessee and Washington DC, however, reported aggregate data on the number of adult and pediatric nonsexual contacts.
Together, the jurisdictions reported 278 mpox cases, and 662 nonsexual case contacts were identified through contact tracing.
Among 563 nonsexual close contacts in Washington, 9 experienced symptoms of mpox in the 21 days following exposure, for a secondary attack rate of 1.6%. Of the 9, 5 had received post-exposure mpox vaccine before symptom onset.
Of the nonsexual contacts, 40.9% were exposed at large gatherings, such as festivals; 12.6% were exposed at places of employment; and 7.8% at home. More than 21% of exposures were in unknown settings.
In Tennessee, 99 nonsexual contacts were identified, with 1 person developing symptoms within 21 days of contact (secondary attack rate, 1.0%). That person also had received post-exposure vaccination.
The secondary attack rate reported from this investigation is consistent with that reported among nonsexual contacts in regions with endemic mpox.
"The secondary attack rate reported from this investigation is consistent with that reported among nonsexual contacts in regions with endemic mpox," the authors concluded. "Monitoring of nonsexual contacts for mpox signs and symptoms is warranted after a known exposure to an mpox patient."
Fractional vaccine dose yields good antibody levels
In other mpox news, a letter today in the New England Journal of Medicine shows that antibody levels against mpox virus after Jynneos vaccination were similar among vaccine recipients regardless of whether they received vaccine dose smaller than that approved by the US Food and Drug Administration (FDA), the injection was between layers of the skin rather than by the standard route under the skin, and regardless of HIV status.
The findings come from the New York City Observational Study of Mpox Immunity, which has followed 145 participants without previous mpox who received either the intradermal or subcutaneous Jynneos vaccine.
Of the study participants 24% were people with HIV, 20% had received previous smallpox vaccination, 89% were LGBTQ+ (of whom 85% were men), and 37% were from underrepresented communities, the authors said.
The smaller doses, about one-fifth the usual dose and spread out by as long as 3 months, were designed to stretch the short supply of vaccine available after the outbreak began in May 2022. The researchers detected mpox-specific immunoglobulin G (IgG) antibodies in some patients more than 6 months after the second (final) dose of the vaccine.
Our study shows that smaller vaccine doses of mpox vaccine administered in two doses, spread out over weeks to months, were similar to the full (subcutaneous) FDA-approved dose.
"Our study shows that smaller vaccine doses of mpox vaccine administered in two doses, spread out over weeks to months, were similar to the full (subcutaneous) FDA-approved dose," said first author and infectious disease specialist Angelica Cifuentes Kottkamp, MD, in a New York University news release. "Implementing the smaller dose was a good emergency measure in the face of immediate shortages of the vaccine."
Participants who had received previous smallpox vaccination had a higher level of antibody titers through 3 months after the second dose of vaccine, but antibody titers were similar regardless of vaccine administration and HIV status.
In participants without a history of smallpox vaccination, IgG titers decreased following the second dose of vaccine (antibody half-life, 107.9 days, with wide confidence intervals).
"The IgG data through 3 months suggest a need for studies to determine whether booster vaccination may be needed for longer-term immunity and the correlation of the antibody titer with vaccine protection," the authors concluded.