Sep 13, 2011
Lab infection suspected at University of Chicago facility
The University of Chicago is investigating a possible lab-acquired infection in a researcher who was hospitalized with a Bacillus cereus skin infection after working with the agent in one of the institution's labs, ScienceInsider, the online news service of Science magazine, reported yesterday. The lab the woman worked in is in the same area where a researcher 2 years ago contracted a fatal plague infection, according to the report. The university said the woman was working on a project led by Dr Olaf Schneewind in a biosafety-level (BSL) 2 lab. She was hospitalized on Aug 27, where she underwent surgery and was treated with antibiotics. The university has suspended work at the lab to decontaminate the area, which is expected to reopen later this week. A University of Chicago official told ScienceInsider that the B cereus work was being conducted with BSL-3 practices and that the woman wasn't studying the pathogen, but might have touched a colleague's spilled inoculant with a gloved hand and touched an uncovered wound on her skin. The official said the school takes the two incidents very seriously, is moving the B cereus work to a BSL-3 lab in another facility, and is rethinking its safety procedures.
Sep 12 ScienceInsider story
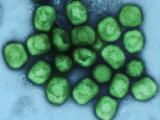
H5N1 hits poultry in Cambodian villages
Cambodia's agriculture ministry yesterday reported an H5N1 avian influenza outbreak among poultry in Banteay Meanchey province, located in the northwestern part of the country. The outbreak began on Aug 25 and killed 156 poultry in the affected villages. Authorities culled 80 more birds—50 chickens and 30 ducks—to control the spread of the virus. In July Cambodia reported a larger outbreak in the same province.
Sep 12 OIE report
Hospitalizations for cholera in Haiti drop 57%
Haiti has seen a large drop in the number of people seeking treatment for cholera, according to an Associated Press (AP) story yesterday. Boston-based Partners in Health said hospitalization rates fell 57% at its 15 cholera treatment centers from July to August, bringing caseloads to pre–rainy season levels. Still, the group said, the 5,400 hospitalizations it recorded in August are a reminder that cholera is still having a significant impact on the country. Haiti's Health Ministry has confirmed almost 440,000 cases and more than 6,200 deaths since the outbreak began last fall.
Sep 12 AP story
ECDC warns of highly drug-resistant bacteria in hospitals
Transferring patients between hospitals, and particularly between countries, raises the risk of spreading highly drug-resistant bacteria called carbapenamase-producing Enterobacteriaceae (CPE), according to a technical report today from the European Centre for Disease Prevention and Control (ECDC). ECDC Director Dr. Marc Sprenger said in a press release, "Our risk assessment highlights that without proper infection control, such as active screening of patients who are transferred across borders and taking additional precautions for the care of patients found to be infected with highly resistant bacteria, such as [CPE], doctors will increasingly face the dilemma of not having any treatment options left." To lower the risk, the agency recommends (1) early rectal screening, (2) added precautions in CPE patient care such as disposable gloves and gowns, (3) cohort nursing, and (4) closer monitoring of cross-border patients. The ECDC also said it supports prudent use of antibiotics. The report is based on a review of the literature and findings of a 10-member expert panel that convened last November. Enterobacteriaceae is a large family of bacteria that includes Klebsiella species.
Sep 13 ECDC report
Sep 13 ECDC press release
Hospital-acquired infections much more common in developing nations
In spite of "remarkably similar" prevention efforts, the rate of hospital-acquired infections in developing nations is dramatically higher than in the United States, according to surveillance data from 36 countries in Latin America, Africa, Europe, and Asia. The study, conducted by the International Nosocomial Infection Control Consortium from January 2004 through December 2009 in 422 intensive care units in the 36 countries, found 6.8 central line–associated bloodstream infections per 1,000 days of use, compared with a US rate of 2.0. In addition, ventilator-associated pneumonia cases numbered 15.8 per 1,000 ventilator-days, compared with 3.3, and catheter-associated urinary tract infections were almost double: 6.3 vs. 3.3 per 1,000 catheter-days. The study also showed disparities in the prevalence of drug-resistant pathogens: Pseudomonas aeruginosa isolates resistant to imipenem, 47.2% vs 23.0%; Klebsiella pneumoniae isolates resistant to ceftazidime, 76.3% vs 27.1%; Escherichia coli isolates resistant to ceftazidime, 66.7% vs 8.1%; and Staphylococcus aureus isolates resistant to methicillin, 84.4% vs 56.8%.
Sep 12 Am J Infect Control abstract