The European Centre for Disease Prevention and Control (ECDC) reported today that 67 cases of botulism linked to a weight loss procedure have been reported in Turkey and three other European countries.
The 67 cases of the neuroparalytic illness have all been linked to intragastric injection of the botulism neurotoxin (BoNT), with 53 cases reported in Turkey, 12 in Germany, and 1 each in Austria and Switzerland. The patients had the procedure from February 22 to March 1, and among the 63 patients with information, 60 were treated at a private hospital in Istanbul and 3 at a hospital in Izmir. The relevant departments of both hospitals have had their activities suspended.
Symptoms range from mild to severe, with several of the patients hospitalized and a number reportedly admitted to intensive care units and treated with botulinum anti-toxin.
BoNT products, such as Botox, are derived from the bacterium Clostridium botulinum and are commonly used for cosmetic purposes. The ECDC said investigation by Turkish authorities found that licensed BoNT products were used in the procedures, but that these products are not approved for the treatment of obesity by intragastric injection. Excessive doses of BoNTs can cause botulism.
The ECDC is warning European Union/European Economic Area citizens to avoid intragastric treatments with BoNT for obesity in Turkey.
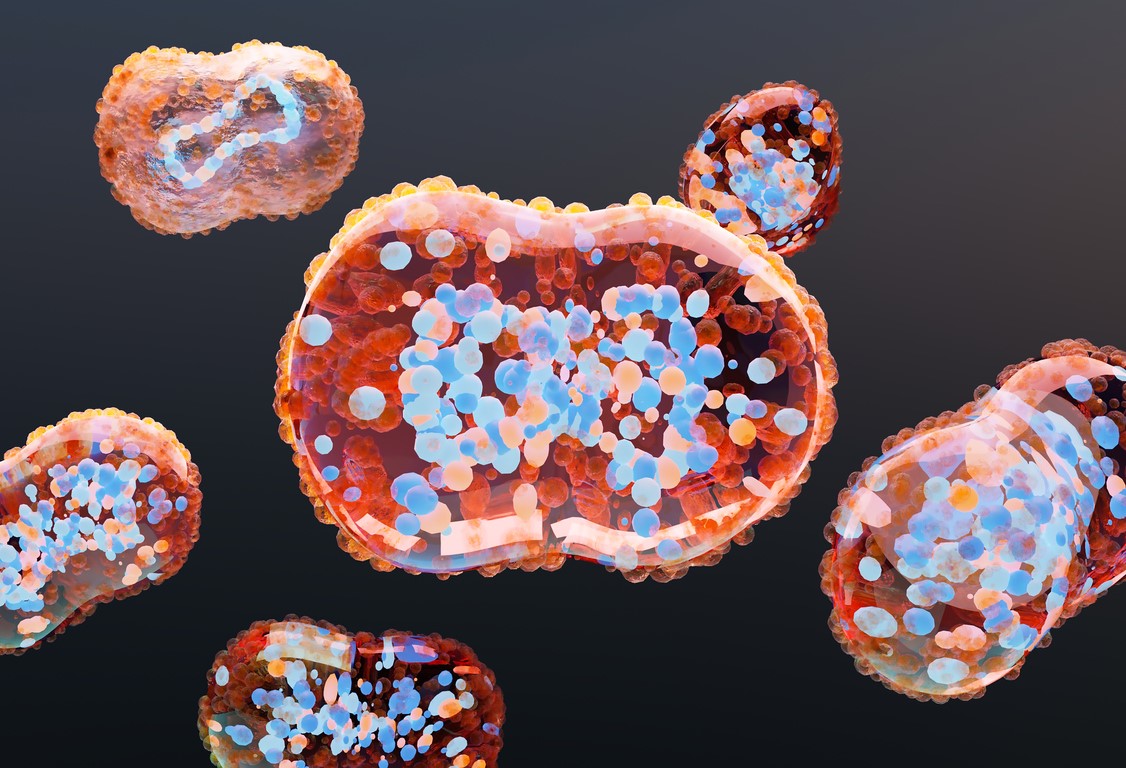 Estimated vaccine effectiveness (VE) of a single dose of the Jynneos attenuated smallpox/mpox vaccine against symptomatic mpox infection was 78% at least 14 days later, according to a
Estimated vaccine effectiveness (VE) of a single dose of the Jynneos attenuated smallpox/mpox vaccine against symptomatic mpox infection was 78% at least 14 days later, according to a 











