A new report of foodborne illness surveillance in the United States shows the country is not meeting disease-reduction goals. That may be, however, because of increased use of culture-independent diagnostic tests (CIDTs), which allow for diagnoses of infections that previously would not have been reported.
A summary of the 2023 Foodborne Diseases Active Surveillance Network report was recently published in Morbidity and Mortality Weekly Report, and the authors said continued surveillance is needed to monitor the impact of changing diagnostic practices on disease trend.
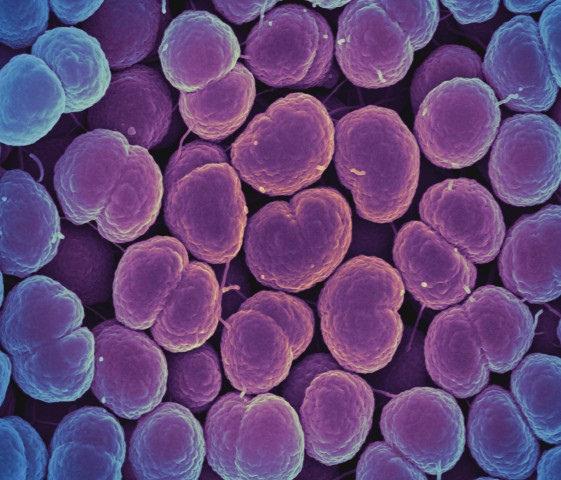
The report is meant to compare 2023 incidences of foodborne illnesses with an annual baseline in 2016 through 2018 as part of the Healthy People 2030 initiative, which outlines disease reduction goals for Campylobacter, Listeria, Salmonella, and Shiga toxin–producing Escherichia coli (STEC) infections.
Testing increased in past decade
In 2023, FoodNet identified 29,607 infections, 7,234 hospitalizations, and 177 deaths overall related to foodborne pathogens.
During 2023, the incidence of domestically acquired campylobacteriosis, STEC infection, yersiniosis, vibriosis, and cyclosporiasis increased, whereas those of listeriosis, salmonellosis, and shigellosis remained stable.
"Increased use of CIDTs facilitates prompt clinical diagnosis and treatment but also complicates the interpretation of surveillance data and trends because CIDT adoption has varied over time, among clinical labs, and by pathogen," the authors wrote.