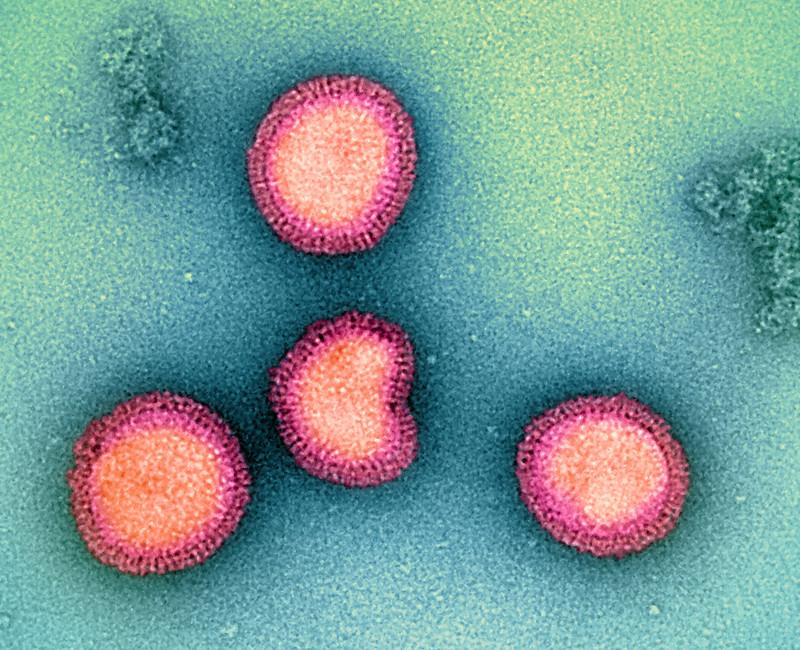
Cidara Therapeutics, Inc announced it has received up to $339 million from the Biomedical Advanced Research and Development Authority (BARDA) to fund work on CD388, a non-vaccine preventive for both pandemic and seasonal flu.
"A long-acting, universal influenza preventative that confers broad protection against all strains of influenza across all populations is critical for pandemic preparedness, especially for the millions of Americans who are immune-compromised, have comorbidities that can lead to severe complications from influenza infection, or the elderly who have diminished response to vaccines," said Jeffrey Stein, PhD, Cidara president and CEO, in a press release. "We welcome BARDA's partnership that will enable us to accelerate domestic supply options for CD388 production."
CD388 not reliant on immune response
Cidara said the funding will help accelerate domestic supply options for CD388 production in the United States.
CD388 is an investigational drug-Fc conjugate (DFC). DFCs are not vaccines or monoclonal antibodies. Instead, the drugs are low-molecular-weight biologics designed to function as long-acting small molecule inhibitors. CD388 is being developed to offer season-long protection against multiple flu strains via a single subcutaneous or intramuscular administration.
Because CD388 is not a vaccine, its activity is not reliant on an immune response.
"Because CD388 is not a vaccine, its activity is not reliant on an immune response and thereby is expected to be efficacious in individuals regardless of immune status," Cidara said. In July the company presented data showing that the drug may protect adults from flu better than flu vaccines.