The latest lab findings on samples collected during an investigation into a febrile illness outbreak in a remote district of the Democratic Republic of the Congo (DRC) reveal common respiratory viruses and falciparum malaria, the World Health Organization (WHO) said in a December 27 outbreak update.
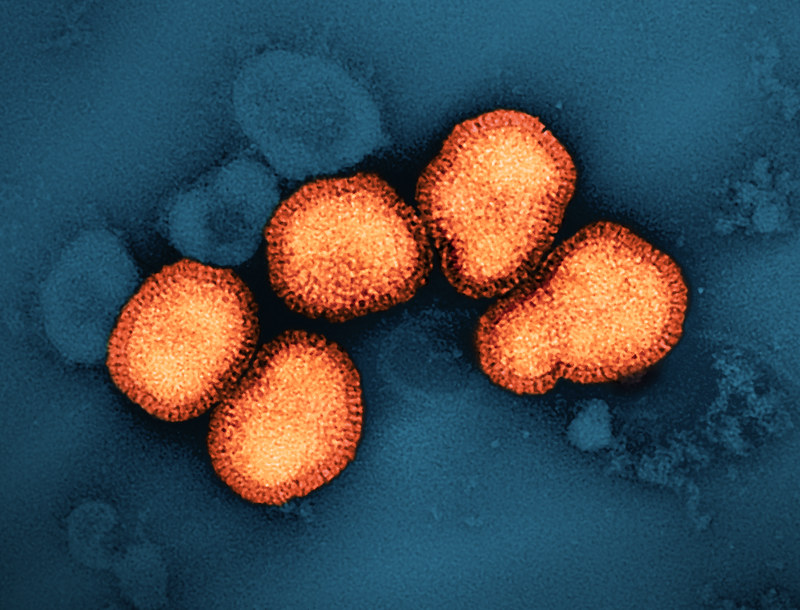
A total of 430 samples were collected from patients with suspected infections in the Panzi health zone, and initial rapid tests and fever panel tests were positive for malaria in 62% and 65% of samples, respectively. Of 89 other samples tested at the INRB in Kinshasa, 64 were positive for common respiratory viruses, including 2009 H1N1 seasonal flu, rhinoviruses, SARS-CoV-2, human coronaviruses, parainfluenza virus, and adenovirus. Further lab tests are still under way, including virological and bacterial analysis.
The WHO now refers to the outbreak as acute respiratory infections complicated by malaria. Officials said acute malnutrition led to an increase in severe illnesses and deaths.
Cases rise, but deaths remain stable
During the investigation, outbreak responders cast a wide net to identify potentially related cases, which resulted in a rapid increase in cases that met the case definition. As of December 16, 891 cases were reported, 48 of them fatal. However, deaths have remained relatively stable.
Cases have remained steady, except for the week ending December 15, which the WHO said may be partly due to increased illness transmission during the rainy season but likely reflects increases in surveillance and case finding. “Notably, the increase in cases is not matched with a comparable increase in deaths," the update said.
The WHO assessed the risk to the affected community as high, requiring efforts to reduce deaths from infections, reduce malnutrition, and improve malaria control. It said the risk to the DRC, region, and rest of the world is low due to the localized nature of the outbreak.














