.jpg)
The World Health Organization (WHO) yesterday released a roadmap to address rising resistance to treatments for HIV, hepatitis B and C, and sexually transmitted infections (STIs).
Building on the WHO's Global Action Plan on Antimicrobial Resistance, the integrated drug resistance action framework proposes a unified global approach to prevent the emergence and spread of drug resistance and reduce its impact through a people-centered approach. The document outlines strategic priorities and concrete actions across five key domains: prevention and response; monitoring and surveillance; research and innovation; laboratory capacity; and governance.
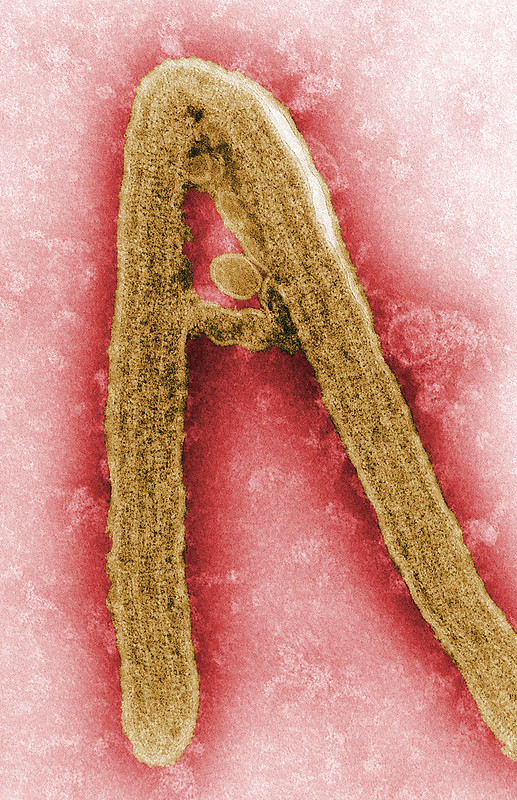
Current treatments for HIV, STIs, and hepatitis B and C face varying degrees of resistance. Among HIV patients with unsuppressed viral load, resistance to dolutegravir-based antiretroviral therapy has been reported in some low- and middle-income countries, with resistance rates ranging from 5% to 20%. Resistance to first-line treatments for Neisseria gonorrhoeae—one of the four most common STIs globally—have substantially increased over the past decade, leaving some gonorrhea patients with limited treatment options.
And while WHO-recommended treatments for hepatitis B and C remain highly effective, there are concerns about emerging resistance amid expanded treatment access.
Rising resistance could undo decades of progress
WHO officials say drug resistance could lead to rising rates of new infections and treatment failure, increase preventable morbidity and mortality, undo decades of progress in HIV, hepatitis, and STI control, and undermine global elimination goals.
“This framework is a call to action for countries, communities and partners to unite around a shared agenda,” Tereza Kasaeva, MD, PhD, director of WHO’s Department for HIV, Tuberculosis, Hepatitis and Sexually Transmitted Infections, said in a news release. “Together, we can preserve the effectiveness of life-saving antimicrobial drugs and accelerate progress toward ending these epidemics.”