Investigations into human and animal infections caused by multidrug-resistant bacteria in Massachusetts reveal genetic links that hint at potential transmission between pets and their owners, researchers reported last week in Clinical Infectious Diseases.
The paper describes two separate investigations that were ultimately linked through epidemiologic and molecular detective work. One investigation began at a veterinary teaching hospital in Worcester County, Massachusetts, where a cluster of carbapenemase-producing Escherichia coli infections were detected in cats and dogs in late 2022, a first for the practice. The other involved a cluster of human infections that occurred months later in the same county, caused by the same bacteria.
For months, there were no known links between the two investigations. But molecular analysis of bacteria samples from the two investigations eventually uncovered links that would reveal a hidden One Health connection.
"Once we put the isolates into the same database, that's when we discovered that they all clustered together," coauthor Stephen Cole, DVM, an assistant professor of clinical microbiology at the University of Pennsylvania's School of Veterinary Medicine, told CIDRAP News.
A growing veterinary problem
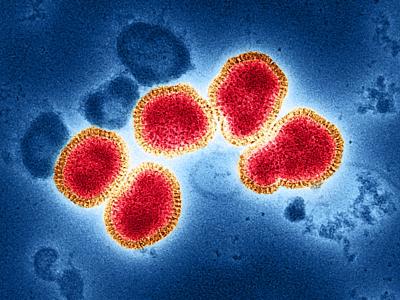
Carbapenemase-producing Enterobacterales (CPE) are multidrug-resistant pathogens that are known to primarily cause difficult-to-treat and sometimes deadly infections in hospital patients.
They've been labeled a high-priority pathogen by both the World Health Organization and the US Centers for Disease Control and Prevention (CDC). A recent report by the CDC highlighted the increase in CPE hospital infections in the United States over the last 5 years, with a dramatic increase observed in CPE-carrying NDM (New Delhi metallo-beta-lactamase) genes.
But there is concern that CPE have begun to spread beyond hospitals and into community settings, because the carbapenemase enzymes that inactivate carbapenem antibiotics are carried on mobile genes that can be shared between bacterial strains and species, enabling increased transmission. There have also been sporadic reports of pets with CPE colonization and infections.
Coauthor Ian DeStefano, DVM, an assistant clinical professor at Tufts University's Cummings School of Veterinary Medicine who was involved in the veterinary investigation, said he believes CPEs are an emerging problem in veterinary medicine. But the average veterinarian knows little about them and has likely never come across one.
"I think there are also instances where vets find isolates that probably are CPEs and just don't know that's what they're looking at," he said.
At the veterinary teaching hospital where the CPE outbreak was identified, further investigation conducted in coordination with the Massachusetts Department of Public Health (MDPH) identified environmental contamination on hospital surfaces and colonization in hospitalized animals.
Once we put the isolates into the same database, that's when we discovered that they all clustered together.
Isolates from hospital surfaces, dogs, and cats were then sent to Cole and colleagues at the University of Pennsylvania's Carbapenem Resistant Enterobacterales Animal Testing and Epidemiology (CREATE) lab for further testing. Whole-genome sequencing (WGS) of the isolates was performed by the Minnesota Department of Health.
Months later, a separate investigation by the Massachusetts State Public Health Laboratory was undertaken to examine potential links between two people who had urinary tract infections caused by the same type of CPE identified at the veterinary hospital—blaNDM-5-harboring E coli—and a third who was colonized with the bacteria. The three case-patients (a 79-year-old woman, a 63-year-old man, and a 23-year-old woman) all lived in Worcester County but had no epidemiologic links such as common healthcare exposure, recent foreign travel, or medical tourism.
"There seemed to be three human isolates that were super related to one another, but it was unclear how the people were," DeStefano said.

The answer became clear after the sequenced isolates from the two investigations were uploaded to the National Center for Biotechnology Information (NCBI) Pathogen Detection database and the results were analyzed at the CREATE lab. The human, animal, and environmental isolates all clustered within 0 to 10 single-nucleotide polymorphisms—an indication they were highly related to one another.
"There was a whole-genome sequencing project over here on people and another over here on animals," said Cole. "And our ability to data share really helped us identify this sort of cryptic connection between the two that you wouldn't have found without doing that."
Though initial interviews of the three patients with CPE infections failed to identify any epidemiologic links between them, the sequencing results prompted follow-up interviews, which found that all three patients had pets in their homes who had received care at the veterinary hospital in the months leading up to their infections.
Although the animals were never screened for CPE, DeStefano said the genetic results, interviews, and timeline of events indicate they had received care at the veterinary teaching hospital when it was experiencing its CPE outbreak. They likely became colonized with the bacteria at the hospital and then spread it to their owners.
"The timeline fits with them being hospitalized at the same time that we were having a CPE problem, and that predated the pet's owner then becoming sick or having some sort of CPE isolate later found," DeStefano said. He also noted that, since transmission can go both directions, it's possible that the CPE outbreak at the veterinary hospital originated with a pet whose owner was colonized with CPE.
"To me, it's the definition of One Health," he added.
Collaboration needed across human, veterinary health sectors
Previous studies have suggested the potential for transmission of resistant bacteria between companion animals and their owners. A 2019 study that analyzed bacteria samples from Dutch pet owners and their pets found a handful of households where drug-resistant E coli isolates carried by dogs and their owners were nearly identical.
But Cole says most of those studies involve colonization and often lack epidemiologic context. Their paper, on the other hand, describes a targeted investigation that revealed the hidden epidemiology behind clinically relevant bacteria that were causing infections. And both he and DeStefano believe that it highlights the need for the human and veterinary health sectors to work together to limit the spread of a significant public health threat.
"Given the contact between large numbers of animals at dog parks, veterinary hospitals, and boarding facilities, the potential for amplification of pets and humans exposed [to CPE] is significant and could result in sporadic cases, clusters, or outbreaks," they and their colleagues wrote in the paper.
To me, it's the definition of One Health.
What would this look like in practice? For one, it would require more real-time surveillance of CPE in veterinary settings and the environments that pets and their owners share and collaborations between state public health departments and animal health authorities to leverage testing infrastructure. They also suggest that human health practitioners include companion animals when considering possible sources of drug-resistant infections.
"We know that this is not an isolated incident, and unfortunately, I don't see this problem going away," said DeStefano.
That sentiment is shared in an accompanying editorial by researchers from the University of Bern in Switzerland, who say the findings from this investigation and others "underscores an alarming One Health concern from the veterinary clinics which needs to be addressed rapidly."
"Incremental efforts across this and other sectors may contribute to curbing the rapid dissemination of CPE into the human and animal populations and prevent the uncontrolled rise of avoidable infections," they wrote.
Although he acknowledges that such efforts will require a level of funding and support for public health that's currently in short supply in most states, Cole said he sees a "golden opportunity" to protect human and animal health.
"We know pets help us live happier, healthier lives in general," he said. "So AMR [antimicrobial resistance] is not just a threat to the health of people, it's a threat to the health of our pets, too. And we can combat it."