The Centers for Disease Control and Prevention (CDC) recently announced that it is monitoring a newly identified SARS-CoV-2 variant called BA.2.87.1 from South Africa that has mutations that may pose a risk of immune escape, but so far there's no sign that it is spreading widely.
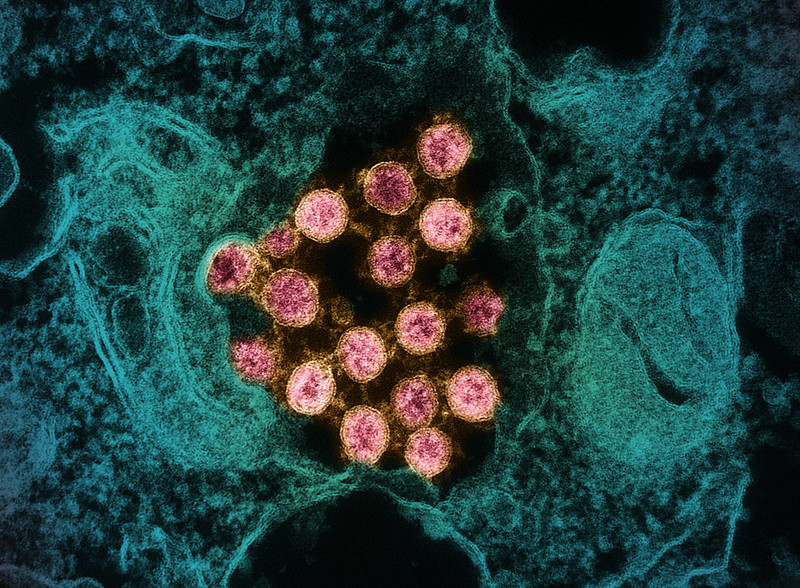
South African scientists have identified nine BA.2.87.1 sequences in samples that were collected between September and December of 2023. No cases have been identified outside of South Africa. "The fact that only nine cases have been detected in one country since the first specimen was collected in September suggests it does not appear to be highly transmissible – at least so far," the CDC said in a February 9 statement.
South African cases reported from three provinces
In South Africa, though, the cases were reported from three provinces over 3 months, suggesting that BA.2.87.1 can spread among people, the CDC said.
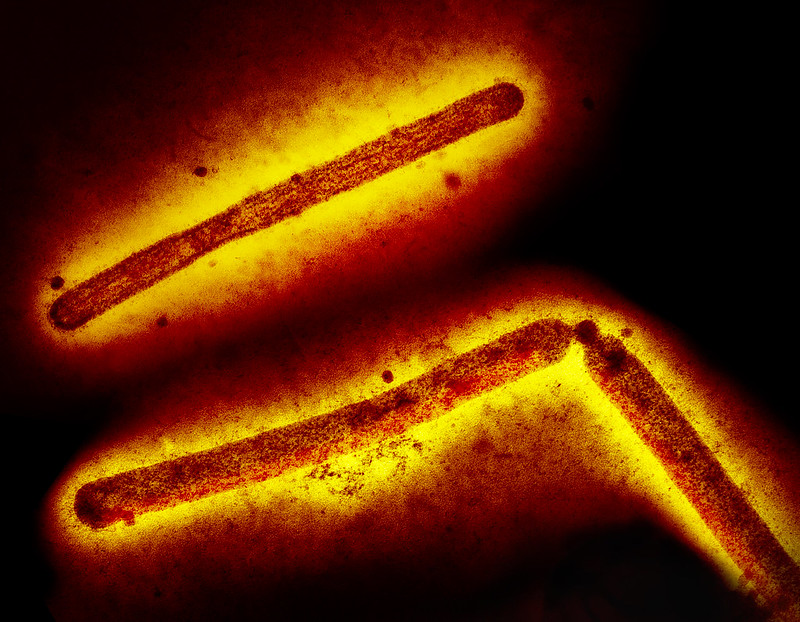
The CDC said it is monitoring BA.2.87.1 because it has more than 30 changes in the spike protein compared to XBB.1.5, the variant covered by the current monovalent vaccine. The CDC said variants with multiple spike protein changes could increase the potential for immune escape from earlier infection or vaccination. Experience with BA.2.86 and its JN.1 offshoot was a reminder that a variant's ability to transmit can change quickly over time.
BA.2.87.1 isn't fueling a detectable increase in South Africa's COVID cases, the CDC said. So far, it's not clear how well the current vaccine would protect against BA.2.87.1, but the group added that recent experience with the JN.1 variant suggests that the current COVID vaccine can help protect against a diverse range of variants.
The European Centre for Disease Prevention and Control (ECDC) is also tracking BA.2.87.1 as a variant under monitoring (VUM).