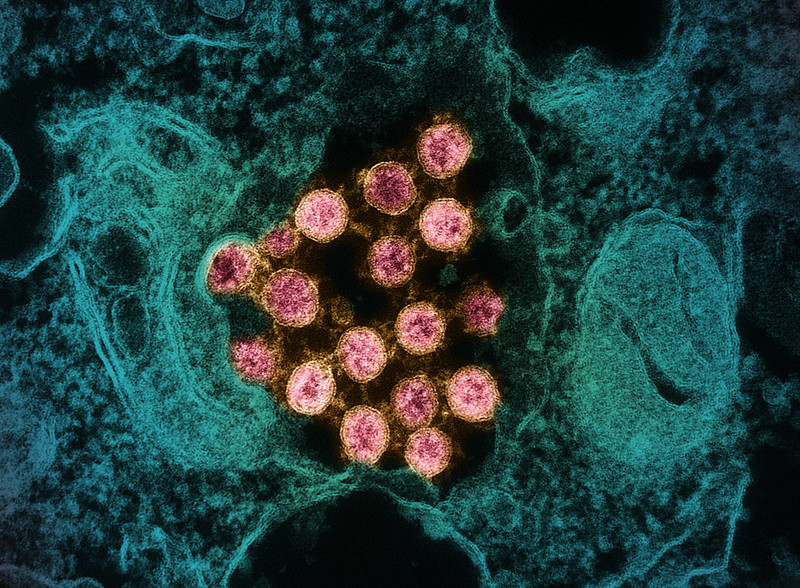
An observational study in eClinicalMedicine suggests that the antiviral drugs azvudine and nirmatrelvir/ritonavir (Paxlovid) were similarly ineffective in preventing death in elderly patients hospitalized for COVID-19 in China, although the authors acknowledge that the findings may be subject to confounding factors and bias.
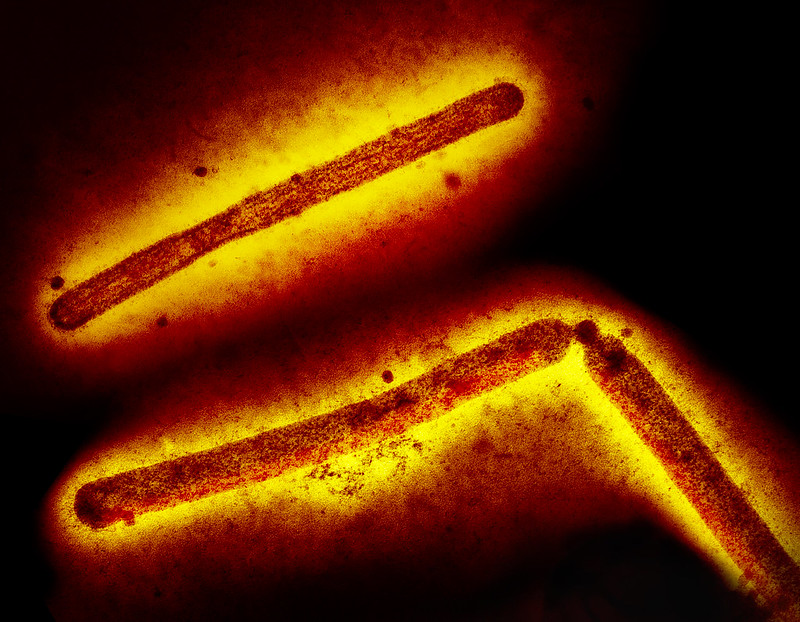
Azvudine has conditional approval for treatment of viral diseases such as COVID-19 and AIDS in China but isn't approved for use in the United States, where Paxlovid is approved for treatment of mild or moderate COVID-19 in high-risk adults.
Researchers from the Chinese PLA General Hospital in Beijing evaluated the electronic medical records of 249 COVID-19 patients with an average age of 91.4 years hospitalized in December 2022 and January 2023. Of all patients, 128 received azvudine, 66 were given Paxlovid, and 55 received no antiviral. Average follow-up was 84 days.
"The proportion of severe illness and death caused by COVID-19 among the elderly is the highest among all age groups, and elderly patients are commonly accompanied by multi-disease and multi-reuse drugs," the study authors noted, adding that caution must be taken when prescribing drugs for these patients.
Potential confounding factors, bias
A total of 77 patients (31%) died during follow-up. Neither antiviral demonstrated a survival benefit, with a Cox analysis of all-cause death showing a 0.73 risk of death in the azvudine group and 0.80 in Paxlovid recipients compared with no antiviral treatment.
The proportion of severe illness and death caused by COVID-19 among the elderly is the highest among all age groups, and elderly patients are commonly accompanied by multi-disease and multi-reuse drugs.
The researchers noted several potential reasons for the lack of clinical benefit, including the advanced age, chronic illness burden, and disease severity among participants and inadequate study power to detect differences.
"Finally, the cause of selection bias cannot be ruled out because patients with more severe clinical presentations may have been preferentially selected by clinicians to receive nirmatrelvir/ritonavir," they wrote. "In that case, patients who received nirmatrelvir/ritonavir would be expected to have worse outcomes, which could obscure a potential therapeutic benefit of nirmatrelvir/ritonavir."