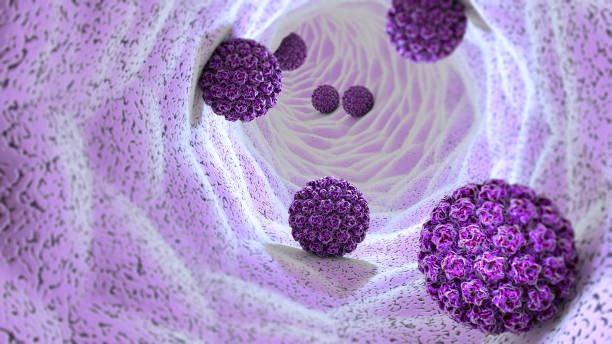
A large-scale randomized controlled trial from Costa Rica finds that one dose of either a bivalent (two-strain) or nonavalent (nine-strain) human papillomavirus (HPV) vaccine provides the same protection against infection with the HPV16 or HPV18 types as the more common two-dose series, offering a potentially transformative tool for global cervical cancer prevention.
HPV types 16 and 18 cause more than 77% of cervical cancers worldwide.
The study, published today in The New England Journal of Medicine (NEJM), enrolled 20,330 girls ages 12 to 16 years old and followed up with them for five years. The rate difference between one and two doses of the bivalent vaccine was −0.13 infections per 100 participants, and the difference between one and two doses of the nonavalent vaccine was 0.21 infections per 100 participants. In all four trial groups, the vaccine was 97% effective, and protection did not wane during the follow-up period.
“This is a very large study, and they evaluated a one-dose vs two- dose strategy for two different versions of the HPV vaccine,” Kevin Ault, MD, an obstetrician-gynecologist at the Western Michigan University Homer Stryker MD School of Medicine and author of several articles on the HPV vaccine, told CIDRAP News. “This study found very high efficacy in all the groups, so one dose is as good as having two doses.” Ault was not involved in the study.
The trial didn’t identify any safety concerns, a finding that’s in keeping with previous research. The safety profiles of HPV vaccines have been evaluated extensively in hundreds of millions of people, note the study authors.
“Given our current political environment, it's important to emphasize that this [study] had a very, very, very high level of safety in it,” says Mark Einstein, MD, chair of the Department of Obstetrics and Gynecology and Women's Health at Montefiore Einstein in New York. Einstein was likewise not involved in the study.
‘Strongest evidence to date’ for vaccine
Previous trials have shown that a one-dose regimen of the HPV vaccine may be as effective as two- and three-dose regimens, “so it’s not surprising that we're seeing such high levels of what they're calling prevention against persistent infection, which we know is a necessary step to get to cervical cancer,” says Einstein.
Eighty-five percent of cases and 90% of deaths from cervical cancer occur in low- and middle-income countries, where access to screening and treatment is limited, and cost is a barrier.
In an NEJM editorial accompanying the study, Ruanne Barnabas, MB, ChB, DPhil, of Massachusetts General Hospital and Harvard Medical School, describes the findings as “the strongest evidence to date” to support the World Health Organization (WHO) recommendation that girls and young women up to age 20 get one or two doses of the HPV vaccine.
Cervical cancer is the fourth most common cancer among women, with more than 660,000 new cases and 340,000 deaths in 2022, Barnabas notes. Eighty-five percent of cases and 90% of deaths from cervical cancer occur in low- and middle-income countries, where access to screening and treatment is limited, and cost is a barrier.
“Most cervical cancers occur in places where vaccination is unavailable due to cost,” says Rebecca Perkins, MD, obstetrician and gynecologist and investigator at the Woman, Mother and Baby Research Institute at Tufts Medical Center who wasn’t involved in the study.
But the problem is not limited to low-income regions. Nearly two decades after HPV vaccines were introduced, only 30% of girls ages 9 to 14 worldwide have been vaccinated, according to WHO estimates. Even in high-income countries like the United States, completion rates for multidose regimens remain suboptimal.
“I think in places like the United States, alternative dosing regimens should be discussed,” says Einstein. “Right now, we’re getting very low compliance and completion of the full three-dose series.”
Opportunity to vastly improve cancer prevention worldwide
Single-dose vaccination would help low-, middle- and high-income countries across the globe overcome the challenge of getting people to return for multiple doses and strengthen WHO’s cervical cancer–elimination strategy, which calls for 90% of girls to be fully vaccinated by age 15, 70% of adult women to be screened in their lifetime, and 90% of women with cervical cancer to receive appropriate treatment.