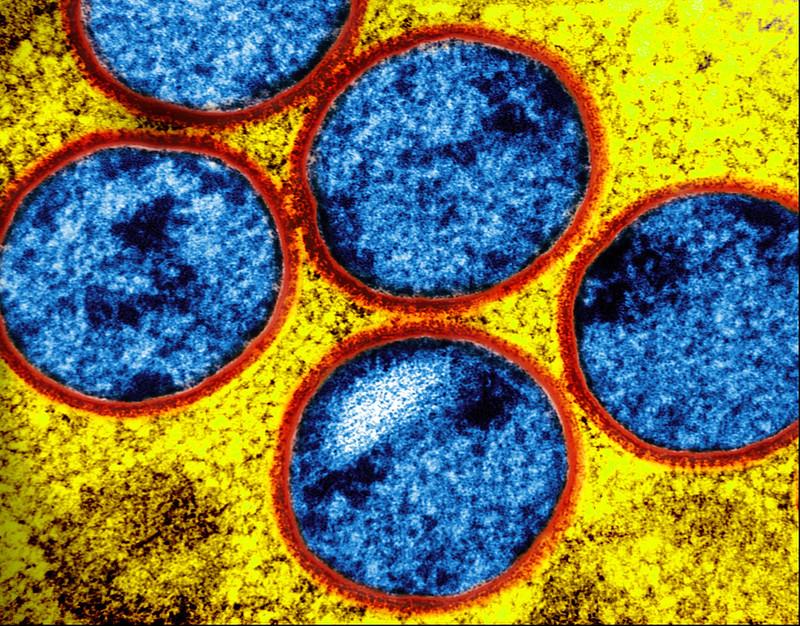
Officials with the California Department of Public Health (CDPH) and local health departments have confirmed a third case in Los Angeles County of the more severe clade 1 mpox infection that was locally acquired, according to a CDPH news release.
Officials say the three recent cases are unrelated. But the fact that all three people had not traveled internationally indicates that local person-to-person spread is likely. The New York Times reports that one patient is from Long Beach and the others are from Los Angeles, which is about 20 miles north.
All 3 patients required hospitalization
All three patients required hospital care and are recovering. "Local health departments and CDPH are conducting enhanced surveillance and contact tracing to identify any additional cases and prevent further transmission," the CDPH said. "At this time, the risk to the general public remains low."
The agency added, "These cases indicate that person-to-person community spread of clade I mpox is occurring in California, primarily impacting communities of gay and bisexual men, and other men who have sex with men, as well as their social networks. Prior cases of clade I mpox in the United States have been associated with international travel to areas where clade I mpox is circulating."
State officials urge people to get both doses of Jynneos mpox vaccine if they or their sex partners may be at risk for mpox.
These cases indicate that person-to-person community spread of clade I mpox is occurring in California, primarily impacting communities of gay and bisexual men.
The US Centers for Disease Control and Prevention reports that six previous US cases of clade 1 mpox involved people who traveled to countries in Central and East Africa that were experiencing clade 1 outbreaks. Those regions have recorded more than 40,000 clade 1 cases. "Both types [clade 1 and clade 2] spread the same way and can be prevented using the same methods," the CDC said.
















