Global deaths from viral hepatitis are rising, despite progress with prevention and better tools for diagnosis and treatment, the World Health Organization (WHO) warned today in its annual hepatitis report, which it released at the World Hepatitis Summit.
New data show that deaths rose from 1.1 million in 2019 to 1.3 million in 2022. Hepatitis is the second-leading infectious disease cause of death, with levels about the same as tuberculosis, another leading cause of infectious disease fatalities.
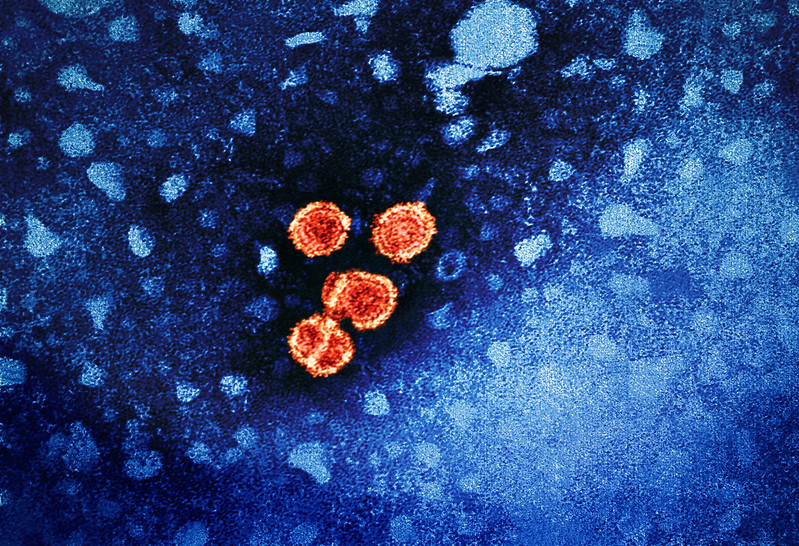
Of hepatitis deaths, 83% were due to hepatitis B, with 17% related to hepatitis C. The WHO estimates that 3,500 people die each day from their hepatitis B or C infections.
The WHO said half of the disease burden is in adults ages 30 to 54, with men accounting for 58% of cases.
Also, disease burden varies by region, with 10 countries making up nearly two thirds of global viral hepatitis cases: Bangladesh, China, Ethiopia, India, Indonesia, Nigeria, Pakistan, the Philippines, Russia, and Vietnam.
Challenges include treatment access, service delivery
Though affordable generic treatments are available, many countries haven't procured them, and problems with access are made worse by pricing disparities and centralized service delivery, the WHO said.
The agency said achieving the elimination goal by 2030 is still possible, and it detailed several steps for accelerating the process, including streamlining service delivery and mobilizing innovative financing.
WHO is committed to supporting countries to use all the tools at their disposal.
In a statement, WHO Director-General Tedros Adhanom Ghebreyesus, PhD, said, "WHO is committed to supporting countries to use all the tools at their disposal—at access prices—to save lives and turn this trend around."














