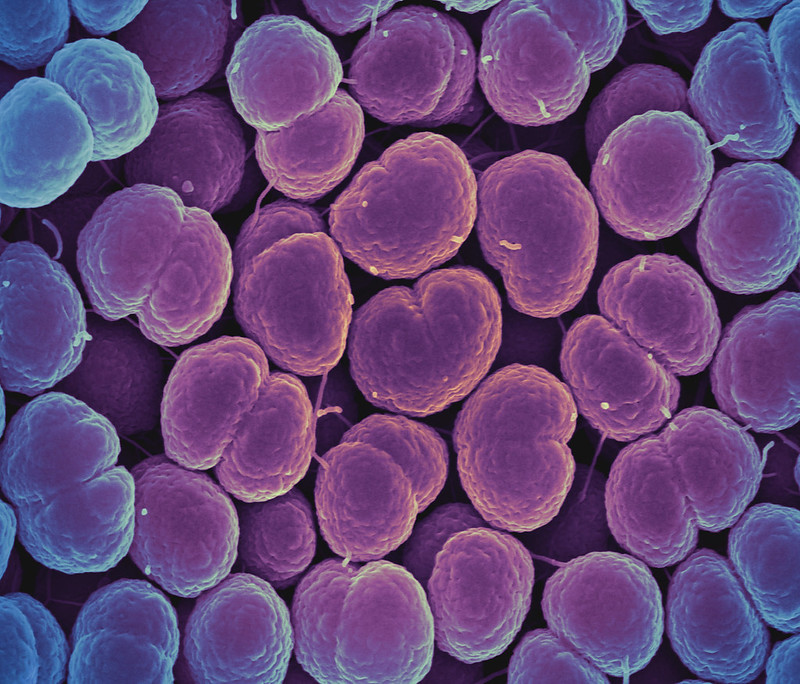
The Food and Drug Administration (FDA) yesterday authorized the first at-home sample-collection test for chlamydia and gonorrhea, the two most common bacterial sexually transmitted infections (STIs). The group notes that levels of both infections are increasing, with an estimated 1.6 million chlamydia cases reported each year, along with more than 700,000 gonorrhea cases.
The Simple 2 Test, from LetsGetChecked, is available over the counter and is indicated for people ages 18 and older. The only other at-home sample-collection test for an STI is for HIV.
After purchasing the test, the user activates the test online and fills out an evaluation for a health provider to review. The user then collects a vaginal swab or urine sample and sends the sample to a designated lab, which delivers the result online, with follow-up from a health provider if results are positive or inconclusive. According to the company's website, patients order STI tests for the two diseases online for $99. The cost of medication, if needed, is not included in the virtual consultation.
The FDA said both infections are easily treated and that home sample collection can help people get quicker results. Jeff Shuren, MD, JD, who directs the FDA's Center for Devices and Radiological Tests, said in an FDA statement, "This authorization marks an important public health milestone, giving patients more information about their health from the privacy of their own home."
_1.jpg)